Abstract
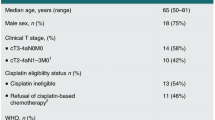
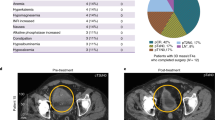
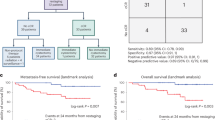
Cohort 1 of the phase 1B NABUCCO trial showed high pathological complete response (pCR) rates with preoperative ipilimumab plus nivolumab in stage III urothelial cancer (UC). In cohort 2, the aim was dose adjustment to optimize responses. Additionally, we report secondary endpoints, including efficacy and tolerability, in cohort 2 and the association of presurgical absence of circulating tumor DNA (ctDNA) in urine and plasma with clinical outcome in both cohorts. Thirty patients received two cycles of either ipilimumab 3 mg kg−1 plus nivolumab 1 mg kg−1 (cohort 2A) or ipilimumab 1 mg kg−1 plus nivolumab 3 mg kg−1 (cohort 2B), both followed by nivolumab 3 mg kg−1. We observed a pCR in six (43%) patients in cohort 2A and a pCR in one (7%) patient in cohort 2B. Absence of urinary ctDNA correlated with pCR in the bladder (ypT0Nx) but not with progression-free survival (PFS). Absence of plasma ctDNA correlated with pCR (odds ratio: 45.0; 95% confidence interval (CI): 4.9–416.5) and PFS (hazard ratio: 10.4; 95% CI: 2.9–37.5). Our data suggest that high-dose ipilimumab plus nivolumab is required in stage III UC and that absence of ctDNA in plasma can predict PFS. ClinicalTrials.gov registration: NCT03387761.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
WES data have been deposited in the European Genome-phenome Archive under accession code EGAS00001004521. WES data and limited anonymized clinical data (baseline characteristics and pathological response) will be made available upon reasonable request for academic use and within the limitations of the provided informed consent by the corresponding author (Michiel S. van der Heijden; ms.vd.heijden@nki.nl) upon acceptance. Requests made through the corresponding author will be answered within 4 weeks and will subsequently be reviewed by the institutional review board of the Netherlands Cancer Institute (NKI-IRB); the researcher will need to sign a data access agreement with the NKI after approval. Proposals for more extensive datasets will be reviewed more extensively by the corresponding authors and the NKI-IRB. Proposals may be submitted from the day of publication up to 36 months after publication. After 36 months, data will be available at the institute’s data warehouse but without investigator support.
Code availability
No custom code or mathematical algorithm was specifically developed for this study. The code related to the RaDaR analysis was locked before study initiation and before analytical validation. This code is proprietary and, as such, cannot be disclosed. However, the outcome of the analytical validation was previously published13 and is further described here as part of the Methods.
Change history
17 July 2023
A Correction to this paper has been published: https://doi.org/10.1038/s41591-023-02500-7
References
Witjes, J. A. et al. European Association of Urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines. Eur. Urol. 79, 82–104 (2021).
Advanced Bladder Cancer Meta-analysis Collaboration. Neoadjuvant chemotherapy in invasive bladder cancer: update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration. Eur. Urol. 48, 202–205; discussion 205–206 (2005).
Pfister, C. et al. Randomized phase III trial of dose-dense methotrexate, vinblastine, doxorubicin, and cisplatin, or gemcitabine and cisplatin as perioperative chemotherapy for patients with muscle-invasive bladder cancer. Analysis of the GETUG/AFU V05 VESPER trial secondary endpoints: chemotherapy toxicity and pathological responses. Eur. Urol. 79, 214–221 (2021).
van Dijk, N. et al. Preoperative ipilimumab plus nivolumab in locoregionally advanced urothelial cancer: the NABUCCO trial. Nat. Med. 26, 1839–1844 (2020).
Rozeman, E. A. et al. Identification of the optimal combination dosing schedule of neoadjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma (OpACIN-neo): a multicentre, phase 2, randomised, controlled trial. Lancet Oncol. 20, 948–960 (2019).
Chalabi, M. et al. Neoadjuvant immunotherapy leads to pathological responses in MMR-proficient and MMR-deficient early-stage colon cancers. Nat. Med. 26, 566–576 (2020).
Vos, J. L. et al. Neoadjuvant immunotherapy with nivolumab and ipilimumab induces major pathological responses in patients with head and neck squamous cell carcinoma. Nat. Commun. 12, 7348 (2021).
Rosenblatt, R. et al. Pathologic downstaging is a surrogate marker for efficacy and increased survival following neoadjuvant chemotherapy and radical cystectomy for muscle-invasive urothelial bladder cancer. Eur. Urol. 61, 1229–1238 (2012).
Stimson, C. J. et al. Early and late perioperative outcomes following radical cystectomy: 90-day readmissions, morbidity and mortality in a contemporary series. J. Urol. 184, 1296–1300 (2010).
Becker, R. E. N. et al. Clinical restaging and tumor sequencing are inaccurate indicators of response to neoadjuvant chemotherapy for muscle-invasive bladder cancer. Eur. Urol. 79, 364–371 (2021).
Powles, T. et al. ctDNA guiding adjuvant immunotherapy in urothelial carcinoma. Nature 595, 432–437 (2021).
Szabados, B. et al. Final results of neoadjuvant atezolizumab in cisplatin-ineligible patients with muscle-invasive urothelial cancer of the bladder. Eur. Urol. 82, 212–222 (2022).
Flach, S. et al. Liquid BIOpsy for MiNimal RESidual DiSease Detection in Head and Neck Squamous Cell Carcinoma (LIONESS)—a personalised circulating tumour DNA analysis in head and neck squamous cell carcinoma. Br. J. Cancer 126, 1186–1195 (2022).
Sharma, P. et al. Nivolumab alone and with ipilimumab in previously treated metastatic urothelial carcinoma: CheckMate 032 nivolumab 1 mg/kg plus ipilimumab 3 mg/kg expansion cohort results. J. Clin. Oncol. 37, 1608–1616 (2019).
Plagnol, V. et al. Analytical validation of a next generation sequencing liquid biopsy assay for high sensitivity broad molecular profiling. PLoS ONE 13, e0193802 (2018).
Gale, D. et al. Development of a highly sensitive liquid biopsy platform to detect clinically-relevant cancer mutations at low allele fractions in cell-free DNA. PLoS ONE 13, e0194630 (2018).
Acknowledgements
We would like to thank all patients and their families who participated in the NABUCCO trial; all staff involved in the care of patients participating in this trial in the Netherlands Cancer Institute; the University Medical Center Utrecht; and the Radboud University Medical Center. We thank the clinical trial teams at participating centers and all staff involved in the collection, processing and storage of trial samples and tumor material. We thank A. Gil-Jimenez for processing the DNA sequencing data and C. Blank for input on the trial design. We thank Bristol Myers Squibb for funding the trial (CA209-9Y4) and for providing the study drugs. The KWF Dutch Cancer Society provided institutional funding.
Author information
Authors and Affiliations
Contributions
J.v.D., N.v.D., B.W.G.v.R. and M.S.v.d.H. designed the study and wrote and amended the study protocol. J.v.D., N.v.D. and M.S.v.d.H. were responsible for the coordination and logistics of the trial. M.S.v.d.H. was the principal investigator of the trial in general and for the Netherlands Cancer Institute. B.B.M.S. was the principal investigator for the University Medical Center Utrecht. N.M. was the principal investigator for the University Medical Center Utrecht. J.v.D., N.v.D., J.M.d.F., M.S.v.d.H., K.H., M.v.d.K., B.W.G.v.R., B.B.M.S. and N.M. recruited patients for the trial. J.v.D., N.v.D., J.M.d.F., M.S.v.d.H., K.H., M.v.d.K., B.W.G.v.R., M.L.v.M., T.N.B., B.B.M.S., R.P.M., N.M. and A.G.v.d.H. were involved in patient care for patients in the trial. K.H., M.v.d.K., B.W.G.v.R., R.P.M. and A.G.v.d.H. were involved in patient recruitment and performed surgery. M.L.v.M., L.M.B. and D.v.d.B. were involved in collection, storage and processing of clinical samples. L.M.B. and C.v.S. were involved in isolation and sequencing of DNA samples. C.P., G.M., S.H., T.A., K.M., N.R. and G.J. were involved in RaDaR panel design. C.P., G.M., S.H., K.M., N.R. and G.J. were involved in isolation and processing of ctDNA. J.v.D., M.S.v.d.H., C.P., G.M., S.H., T.A., K.M., N.R. and G.J. were involved in ctDNA data analysis. J.v.D., M.S.v.d.H., C.P. and G.J. drafted the manuscript. J.M.d.F., B.B.M.S., N.M., R.P.M., A.G.v.d.H., B.W.G.v.R. and N.R. made substantial contributions to the final manuscript. All authors reviewed and approved the submitted manuscript. All authors are personally accountable for their own contributions. Raised questions related to the accuracy or integrity of any part of the work were appropriately investigated, resolved and documented. C.P., G.M., S.H., T.A., K.M., G.J. and N.R.: employed by Inivata, Ltd. RaDaR is a United States, European Union and United Kingdom registered trademark of Inivata, Ltd. B.B.M.S.: advisory role (compensated and institutional) with Pfizer, Merck Sharp & Dohme, Bristol Myers Squibb, Novartis and IPSEN; research support (institutional) from Pfizer, Astellas and Bristol Myers Squibb. N.M.: advisory role (compensated and institutional) with Roche, Merck Sharp & Dohme, Bristol Myers Squibb, Bayer, Astellas and Janssen; research support (institutional) from Astellas, Bristol Myers Squibb, Janssen, Pfizer, Roche, Sanofi and Genzyme. J.M.d.F.: advisory role for Merck Sharp & Dohme, Pfizer and Janssen; travel expenses from Pfizer. R.P.M.: advisory role (institutional) with Merck, Merck Sharp & Dohme, Janssen and Bristol Myers Squibb; research support (institutional) from Janssen, Astellas, AstraZeneca, Merck Sharp & Dohme, Bristol Myers Squibb and Roche. A.G.v.d.H.: advisory role with Merck, Pfizer, Janssen, Bristol Myers Squibb, Astellas, AstraZeneca and Merck Sharp & Dohme. D.v.d.B.: expert testimony for Roche Diagnostics; payment or honoraria for lectures, presentations, manuscript writing or educational events from Roche Diagnostics. B.W.G.v.R.: advisory boards with AstraZeneca, Ferring and QED Therapeutics. M.S.v.d.H.: research support from Bristol Myers Squibb, AstraZeneca, Roche and 4SC; consultancy fees from Bristol Myers Squibb, Merck, Roche, AstraZeneca, Seagen, Pfizer and Janssen (all paid to the Netherlands Cancer Institute). All other authors have nothing to declare.
Corresponding authors
Ethics declarations
Competing interests
M.S.v.d.H. received funding, paid to the Netherlands Cancer Institute, from Bristol Myers Squibb to finance the NABUCCO study. No other authors have received financial support for the work in this manuscript, and no medical writer was involved at any stage of the preparation of this manuscript.
Peer review
Peer review information
Nature Medicine thanks Matthew Galsky, Matthew Schipper and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary handling editors: Ulrike Harjes and Saheli Sadanand, in collaboration with the Nature Medicine team.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 NABUCCO study design.
Cohort 1 is shown at the top, cohort 2A and cohort 2B are shown at the bottom. Arrows correspond with timing of study procedures and apply to all cohorts. Peripheral blood mononuclear cells (PBMCs), urine and plasma samples were collected <24 hours prior to corresponding treatment cycle or radical surgery. C1/2/3: first, second and third treatment cycle.
Extended Data Fig. 2 Treatment, response and follow-up details for every patient treated in cohort 2A and 2B.
Swimmer plot with treatment and follow-up details for every patient in cohort 2A and 2B. Patients are organized per cohort and based on inclusion date. Time is relative to the date of first treatment of ipilimumab plus nivolumab (C1). Clinical TNM-stage prior to start of treatment is shown on the left side of the plot. Pathological TNM-stage after surgery is shown on the right side of the plot. Orange and green boxes represent treatment cycles administered. Black dots represent radical surgery. Open circles represent alternative surgery (transurethral resection bladder tumor and pelvic lymph node dissection). Black horizontal lines represent progression-free survival. Vertical lines indicate disease progression. Red horizontal lines represent survival after disease progression. Black cross indicates death. Two fatal surgery-related adverse events occurred within 90 days after surgery, both hemorrhage after an intra-operative complication. After extensive review, no relation with ipilimumab and/or nivolumab was established. Ipi: ipilimumab, Nivo: nivolumab, TURBT: transurethral resection of the bladder tumor, LND: lymph node dissection, C1: first treatment cycle.
Extended Data Fig. 3 Workflow of RaDaR panel generation and ctDNA assessment in plasma and urine.
DNA was isolated from baseline tumor sample and from PBMCs and used for whole-exome sequencing to identify tumor-specific somatic mutations. A personalized ctDNA assay was developed for each patient. Cell-free DNA and buffy coat DNA from EDTA-plasma and urine samples were analyzed together with tumor DNA using the personalized assays to confirm somatic mutations and perform CHIP filtering. PBMCs: peripheral blood mononuclear cells, ctDNA: circulating tumor DNA, CHIP: clonal hematopoiesis of indeterminate potential.
Extended Data Fig. 4 ctDNA assessment in urine and relation to outcome.
Urine was assessed in patients in cohort 1 (n=24). a, Mean eVAF% in urine before and during treatment, and pre-surgery for responders and non-responders (left; baseline: P=0.09; pre-surgery: P=0.33) and for patients with and without a pathological complete response in the bladder (ypT0Nx versus ypTis/Ta/T1-4aNx) (right; baseline: P=0.33; pre-surgery: P<0.01). Boxplots show median value and 25th and 75th percentiles. Whiskers show minimum/maximum values. P-values: two-sided Mann-Whitney test. b, Individual data points for eVAF% in urine before and during treatment, and pre-surgery. Dark blue bars: patients with a pathological complete response (pCR, ypT0N0), light blue bars: patients with no residual muscle-invasive disease (ypTis/Ta/T1N0), red bars: patients with muscle-invasive disease in the bladder (≥ypT2Nx), Mixed dark blue and red bars: patients with a pCR in the bladder and lymph node metastases (ypT0N+), missing bars: missing samples. Undetectable values are plotted as 0.0002. c, Percentage of patients with no detectable ctDNA in urine at latest available sample pre-surgery for patients categorized in different ways. Responders vs non-responders: P=0.39; pCR vs non-pCR: P=0.08; bladder pCR vs bladder non-pCR: P<0.01. P-values: two-sided Fisher’s Exact test comparing the proportion of patients with detectable ctDNA pre-surgery in responders (ypTis/Ta/T1N0) compared to non-responders (left), patients with or without a pCR (ypT0N0; middle) and patients with or without a pathological complete response in the bladder (ypT0Nx; right). d, Progression-free survival for patients with and without detectable ctDNA in urine measured at latest available sample pre-surgery. Hazard ratio (HR) and P-value: Hazard ratio: 0.70; 95% confidence interval: 0.086-5.70; P=0.76 using a two-sided Log-rank (Mantel-Cox) test. ND: not detectable, Pre-C2/3: prior to second or third treatment cycle.
Extended Data Fig. 5 Sankey Diagrams showing the ctDNA dynamics and relation with outcome.
Top: ctDNA in urine in patients in cohort 1 (n=24). Bottom: ctDNA in plasma in patients in cohort 1 and 2 combined (n=41). Red, blue and grey bars represent the number of patients with detectable, undetectable or missing ctDNA measurements, respectively, at different timepoints (Baseline, Pre-C2, Pre-C3 or Pre-surgery). In follow-up, red and blue bars represent the number of patients with and without disease progression, respectively. Pre-C2/3: prior to second or third treatment cycle.
Extended Data Fig. 6 ctDNA assessment in plasma in cohort 2A and 2B.
Patients are organized per cohort, based on highest eVAF% at baseline. Blue bars: responders (ypT0/Tis/Ta/T1N0), red bars: non-responders (≥ypT2 and/or N+), grey bars: non-evaluable patients, missing bars: missing samples. Undetectable values are plotted as 0.0002. ND: not detectable, Pre-C2/3: prior to second or third treatment cycle.
Supplementary information
Supplementary Information
Supplementary Fig. 1, Supplementary Tables 1–3 and NABUCCO Study Protocol
Supplementary Tables 4–6
Supplementary Table 4: WES data; Supplemtary Table 5: Plasma + urine data; Supplementary Table 6: Variants + evaf%
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
van Dorp, J., Pipinikas, C., Suelmann, B.B.M. et al. High- or low-dose preoperative ipilimumab plus nivolumab in stage III urothelial cancer: the phase 1B NABUCCO trial. Nat Med 29, 588–592 (2023). https://doi.org/10.1038/s41591-022-02199-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41591-022-02199-y
This article is cited by
-
Spatial relationships in the urothelial and head and neck tumor microenvironment predict response to combination immune checkpoint inhibitors
Nature Communications (2024)
-
Turning up the heat: CTLA4 blockade in urothelial cancer
Nature Reviews Urology (2024)
-
Bladder cancer
Nature Reviews Disease Primers (2023)
-
Global trends in the epidemiology of bladder cancer: challenges for public health and clinical practice
Nature Reviews Clinical Oncology (2023)