-
Welcome to Celiac.com!
You have found your celiac tribe! Join us and ask questions in our forum, share your story, and connect with others.
-
Celiac.com Sponsor (A1):
Celiac.com Sponsor (A1-M):
-
Get Celiac.com Updates:Support Celiac.com!
Search the Community
Showing results for 'Larazotide' in articles.
-
Celiac.com 02/28/2024 - We get a lot of questions about what celiac disease trials and studies are going on, but there are so many, it can be hard to keep track. One easy source is the Mayo Clinic, which is at the forefront of a number of research trials, and studies to better understand, and treat celiac disease. Currently, there are more than a dozen exciting clinical trials underway, each focusing on different aspects of the celiac disease. One study aims to assess the effect of gluten on gut barrier function by using a novel gut permeability test developed by Mayo Clinic researchers. Another trial is evaluating the safety and tolerability of a potential new treatment, KAN-101, for celiac disease patients. Additionally, researchers are investigating the effectiveness and safety of numerous compounds for relieving symptoms in adult celiac disease patients. These trials represent important steps forward in advancing our understanding of celiac disease and developing new therapies to improve the lives of those affected by this condition. Celiac disease trials and studies currently underway at the Mayo Clinic facilities include: Gut Permeability Assessment in Celiac and Gluten Sensitive Children Rochester, MN This study will assess the effect of gluten on gut barrier function. Investigators at the Mayo Clinic have developed a new gut permeability test using rhamnose (sugar & water solution), and are hoping to prove its effectiveness in a clinical setting. A Study to Assess the Safety and Tolerability of Single and Multiple Doses of KAN-101 in Celiac Disease Patients Rochester, MN The purpose of this study is to assess the safety and tolerable of single and multiple doses of KAN-101 in patients with Celiac disease. A Study to Evaluate the Effectiveness and Safety of Larazotide Acetate for the Relief of celiac disease Symptoms Rochester, MN The purpose of this study is to assess the effectiveness and safety of larazotide acetate versus placebo for the relief of persistent symptoms in adult celiac disease patients. Study of the Safety, Tolerability, Pharmacokinetics and Biomarker of DONQ52 in Celiac Disease Patients Rochester, MN The purpose of this study is to evaluate the safety and tolerability of single and multiple doses of DONQ52 in celiac disease patients and to evaluate the safety and tolerability of DONQ52 in celiac disease patients in the presence of gluten after multiple doses of DONQ52. Furthermore, to characterize the DONQ52 PK profile following single and multiple subcutaneous (SC) dose(s) in celiac disease patients and to investigate the immunogenicity of DONQ52. A Study of the Response to and Changes in Intestinal Permeability 4 hours after a Gluten Challenge in Subjects with Celiac Disease and Non Celiac Gluten Sensitivity Rochester, MN The purpose of this study is to identify mediators—innate immune system and intestinal permeability—of acute onset gastrointestinal symptoms after gluten ingestion in subjects with celiac disease and non-celiac gluten sensitivity. Gut Permeability in Environmental Enteropathy Rochester, MN The goal of this project, to develop a simple and sensitive test of small bowel permeability, will improve the scientific and public health understanding of environmental enteropathy and guide development of preventative and treatment modalities such as clean water and sanitation. Mucosal Interactions in Celiac Disease Rochester, MN To obtain biopsies and blood from subjects not previously known to have celiac disease who are undergoing duodenal biopsies for clinical indications. The subjects will have no prior diagnosis of celiac disease and are eating a gluten-containing diet. The biopsies will be treated “in vitro” with enzymatic digests of gluten derived from bread made from different species of wheat, the auto-antigen tTg, cytokines, or other proteins. A Study to Evaluate the Safety, Effectiveness, and Tolerability of Latiglutenase to Treat Patients with Well-Controlled Celiac Disease Rochester, MN The purpose of this study is to demonstrate a positive correlation of histologic protection (biological signature) and symptom protection (clinical outcome) for latiglutenase treatment versus placebo in Celiac Disease (celiac disease) patients undergoing a deliberate gluten challenge. A Study of the Safety, Pharmacodynamics, Effectiveness, and PK of TIMP-GLIA in Subjects with Celiac Disease Rochester, MN The purpose of this study is to evaluate participants for immune responses and histological changes in the small bowel following 2 doses of TIMP-GLIA or placebo and a 14-day oral gluten challenge. Dose-Ranging Study of the Efficacy and Safety of TAK-101 for Prevention of Gluten-Specific T Cell Activation in Participants With Celiac Disease on a Gluten-Free Diet Rochester, MN The purpose of this study is to compare the number of baseline interferon-gamma (IFN-γ) spot forming units (SFUs) to the number of IFN-γ SFUs after a 6-day oral gluten challenge among HLA DQ2–positive subjects treated with TAK-101 versus placebo. A Study of Simvastatin Metabolism as a Test for Celiac Disease Activity Rochester, MN The purpose of the study is to assess the connection between simvastatin metabolism by an enzyme that varies based on the state of the small intestine in treated celiac disease. Antibody Treatment for Advanced Celiac Disease Rochester, MN Celiac disease is a condition where the immune system attacks the cells of the small intestine. The intestine becomes inflamed and cannot digest food properly. The disease most often causes a reaction to foods that contain gluten. Most people can treat celiac disease with a gluten-free diet. However, some people have digestion problems even on a gluten-free diet. Researchers want to try a new antibody therapy for celiac disease. The treatment may block the immune reaction that causes the disease. They will test this antibody in people who have celiac disease that has not responded to a gluten-free diet. Prospective, Randomized, Double-Blind, Placebo-Controlled, Crossover Study in Symptomatic Celiac Disease Patients Rochester, MN This is a phase 2b, multi-center, prospective, randomized, double-blind, placebo-controlled, crossover study in symptomatic celiac disease patients attempting a gluten free diet (GFD) for at least one year prior to screening. A Study of TAK-062 in Treatment of Active Celiac Disease in Participants Attempting a Gluten-Free Diet Rochester, MN; Scottsdale/Phoenix, AZ The purpose of this study is to see how TAK-062 works to reduce celiac-related symptoms and improve small intestinal damage due to gluten exposure, in participants with celiac disease (celiac disease) attempting to maintain a gluten-free diet (GFD) in treated participants versus placebo controls. A Study of the Safety, Effectiveness and Tolerability of Nexvax-2 in Patients with Celiac Disease (celiac disease) Rochester, MN The purpose of this study is to evaluate the human leukocyte antigen (HLA)-DQ 2.5+ in adults with celiac disease (celiac disease). Evaluation of the Efficacy and Safety of ALV003 in Symptomatic in Celiac Disease Patients Scottsdale/Phoenix, AZ; Jacksonville, FL; Rochester, MN To determine the effects of 12 weeks administration of different dose levels of ALV003 on the mucosal lining of the small intestine and symptoms in celiac disease patients. Minimal Risk Registry of Endoscopic Image and Pathology Correlation for Fujiflim Jacksonville, FL; Rochester, MN The purpose of this study is to see if advanced endoscopic imaging may be helpful to accurately distinguish pathological tissue from normal tissue and guide therapy of endoscopically identified pathology. Functional Gastrointestinal Disease, Celiac Disease, and Non-celiac Gluten Sensitivity in an Olmsted County Cohort Rochester, MN The aim of this study is to the number of individuals following a gluten-free diet and possible reasons including symptoms of non-celiac gluten sensitivity and functional gastrointestinal diseases (FGIDs). lso assess Diagnoses and lab values associated with celiac disease, NCGS, and FGIDs will also be assessed, as well as past GI survey data and medical record data available through the Rochester Epidemiology Project. Stay tuned for updates on the progress of these and other related studies! Read more at Mayo.edu
- 3 comments
-
- celiac disease
- mayo clinic
-
(and 3 more)
Tagged with:
-
Celiac.com 07/18/2022 - Currently, a gluten-free diet is the only treatment for people with celiac disease. A number of companies have been attempting to create treatments that reduce or eliminate celiac disease symptoms, mostly for patients on a gluten-free diet. Larazotide, whose clinical trial is dubbed "CedLara," is such a drug. It's designed to reduce persistent celiac disease symptoms for people on a gluten-free diet. In an earlier phase 2 trial, Larazotide was shown to reduce celiac symptoms in patients who had been on a gluten-free diet for at least 12 months. Many were excited to see how it would do in a phase 3 trial. The answer, unless we get some better news from 9 Meters Biopharma, the company that has been developing it, is badly. For the phase 3 trial, 9 Meters Biopharma set out to enroll 525 patients in the phase 3 trial to determine the effect of larazotide on celiac disease severity. To determine the number of people needed to measure a statistically significant effect, the company conducted an analysis with half of the expected patients enrolled. According to a company news release, their analysis showed that the additional number of patients needed to produce a significant clinical outcome between placebo and Larazotide is too large for the company to pursue. Reading between the lines of the news release, it seems as though the the company might need far more test subject than originally estimated to show a statistically significant result. That means that, no matter how effective the drug was for some people, the company can't afford to test in large enough numbers to show that it's genuinely effective. With the failure of Larazotide, 9 Meters Biopharma announced that it will be pivoting to the development of vurolenatide, a repeated injection aimed at increasing nutrient absorption in patients with short bowel syndrome. Phase 2 results should be unveiled soon. The failure of Larazotide marks the latest addition to the growing graveyard of celiac disease drugs. As Larazotide has been touted since 2013, this failure is particularly disappointing. To punctuate the ignoble end for a once hopeful drug, the company's CEO and president, John Temperato, says that financial and human resources from Larazotide will be reassigned to advance vurolenatide and the company’s early-stage product candidates, pending a review. Read more at digitaljournal.com
- 3 comments
-
- celiac disease
- clinical
-
(and 5 more)
Tagged with:
-

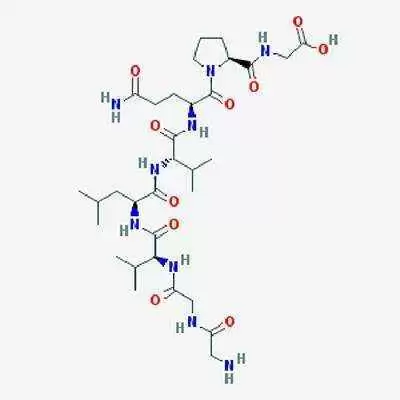
New Developments in Celiac Disease Treatment
Jefferson Adams posted an article in Diagnosis, Testing & Treatment
Celiac.com 12/13/2023 - Celiac disease is a common autoimmune disease affecting more than 1% of the population. In celiac disease, the ingestion of gluten, a protein found in wheat, barley, and rye, triggers an immune response targeting the small bowel. In susceptible individuals, this immune reaction leads to both gastrointestinal and systemic symptoms. Unlike some other autoimmune diseases, the specific immunogenic antigens responsible for the immune response in celiac disease have been identified and extensively characterized. Consequently, a gluten-free diet has long been established as an effective treatment. This is not an easy task, partly due to a lack of awareness of the gluten content in foods, and the extensive incorporation of gluten into many processed foods. Furthermore, a gluten-free diet can impose a sense of limitation, and can be associated with decreased quality of life, in some celiac disease patients. This contributes to gluten contamination in the diets of four out of five celiacs trying to follow a gluten-free diet. Furthermore, one in three adult celiac patients will report persistent symptoms, while two in three will not achieve full histological recovery when on a gluten-free diet. In recent years, extensive research has fueled a quest for a pharmacological treatment for celiac disease, the development of which represents a sort of a Holy Grail for many researchers and patients. A new review presents a concise description of the current rationale and main clinical trials related to celiac disease drug therapy. The review is the work of by Professor Mariana Verdelho Machado, with the Gastroenterology Department, Hospital de Vila Franca de Xira, Nª 2, Vila Franca de Xira, Portugal; and the Clínica Universitária de Gastrenterologia, Faculdade de Medicina, Universidade de Lisboa, Avenida Prof. Egas Moniz, Lisbon, Portugal. Estimates suggest that over 1% of the global population, roughly 80 million people, is affected by celiac disease. The classical presentation involves symptoms of malabsorption, such as diarrhea, weight loss, and nutritional deficits. However, a significant portion of patients either remains asymptomatic or experiences non-specific and extra-intestinal symptoms. Despite the challenges posed by the strict dietary regimen, achieving mucosal healing through a gluten-free diet is crucial, particularly given the increased mortality observed in some cohorts of celiac patients. Challenges with the Gluten-Free Diet The gluten-free diet is currently the only proven effective treatment for celiac disease. However, its implementation presents various challenges. Adherence rates to a strict gluten-free diet fluctuate widely, ranging from 42% to 91%. Moreover, even among those who claim adherence, up to 80% might inadvertently consume gluten due to contamination or non-compliance. Additionally, achieving mucosal healing, a critical aspect of managing celiac disease, appears to occur in less than half of adults following a gluten-free diet. Rationale for Drug Development In the past decade, there has been a concerted effort to explore pharmacological treatments for celiac disease. The endeavor is particularly challenging as a well-established, non-pharmacological therapy— the gluten-free diet—already exists. For a new drug to be a viable alternative, it must demonstrate efficacy, lack significant adverse effects, be simple to administer (preferably orally), and be cost-effective. Pharmacological Treatments in Focus Efforts in drug development for celiac disease have focused on three main scenarios: maintenance therapy, rescue therapy after acute gluten exposure, and mitigation of chronic inadvertent gluten exposure. Larazotide: One drug in clinical research is larazotide, designed to stabilize enterocyte tight junctions, thereby reducing intestinal permeability. While phase 2 studies showed promising results in decreasing symptoms and serological markers, a phase 3 trial in 2022 was suspended after an interim analysis revealed no meaningful effects. Latiglutenase: Another promising drug is latiglutenase, a mix of glutenases. Phase 2 studies demonstrated its efficacy in preventing mucosal degradation and symptom development resulting from gluten contamination. Latiglutenase is considered a strong candidate for becoming a standard adjunctive therapy in celiac disease treatment. IL-15 Pathway Inhibition: For patients unresponsive to a gluten-free diet or those with refractory celiac disease (RCD), research has focused on the IL-15 pathway. While blocking IL-15 with PRN15 showed disappointing results, tofacitinib, a pan-JAK inhibitor acting on the IL-15 receptor signaling pathway, appears promising. Immune Tolerance Induction: Inducing immune tolerance to gluten is an appealing strategy to avoid systemic immune suppression. Strategies like therapeutic vaccines and hookworm infestation, despite initial disappointment, have not been entirely ruled out. Future Prospects and Considerations The ongoing research prompts questions about the role these emerging drugs might play in treating extra-intestinal manifestations associated with celiac disease, such as neuropsychiatric and autoimmune conditions. While these drugs offer hope, they must surpass the effectiveness and safety of the existing dietary therapy, a high bar given the complexity of celiac disease and the challenges posed by gluten exposure. The researchers conclude that celiac disease patients need effective and practical treatment options beyond the stringent gluten-free diet. They also note that ongoing developments in pharmacological treatments bring hope for improved management, especially for patients facing challenges with dietary adherence and inadvertent gluten exposure. However, the complexity of celiac disease demands a meticulous approach to drug development, ensuring not only efficacy and ease of use, but also safety and accessibility. As research progresses, the landscape of celiac disease management may witness transformative changes, offering a brighter outlook for those living with this autoimmune condition. Read more in the Int. J. Mol. Sci. 2023, 24(2), 945.- 3 comments
-
- celiac disease
- development
-
(and 6 more)
Tagged with:
-
Celiac.com 09/29/2020 - Currently, the only medically accepted treatment for celiac disease is a completely gluten-free diet (GFD), which can be both expensive and challenging to maintain. One promising celiac treatment currently in development is larazotide acetate (AT-1001), an anti-zonulin, designed to regulate gut permeability in people with celiac disease. A team of researchers recently conducted a systematic review and meta-analysis of data from all randomized controlled trials (RCTs) assessing the effectiveness and safety of larazotide acetate in celiac patients. The research team included Ahmed Abu-Zaid, Noor Tariq Alhaddab, Razan Abdulkarim Alnujaidi, Hadeel Abdulaziz Alharbi, Fulwah Alangri, Naseem Alyahyawi, Aminah Kamal, Abdulaziz Khalaf Altowairqi, Habeeb Alhabeeb, Sami Almustanyir, and Reem Abdullah Alyoubi. They are variously affiliated with the College of Medicine at Alfaisal University in Riyadh, Saudi Arabia; the Department of Pediatrics at King Abdulaziz University Hospital, Jeddah, Saudi Arabia; the Department of Medicine at the Ministry of Health in Riyadh, Saudi Arabia; the Department of Medicine at the Alhada Armed Forces Hospital in Taif, Saudi Arabia; and the Research Center at King Fahad Medical City in Riyadh, Saudi Arabia. The team began by searching four databases from inception to 20-August-2020 using related keywords to isolate appropriate studies of larazotide acetate in people with celiac disease. The team identified all relevant RCTs and assessed bias risk. They then pooled continuous outcomes as mean difference and dichotomous outcomes as risk ratio with 95% confidence interval under fixed-effects meta-analysis model. They found four RCTs that met the study parameters, which included 465 celiac patients on larazotide acetate, and 161 on a placebo. Three and two studies included data on the results for patients on gluten challenge and GFD, respectively. The total effect estimates showed no substantial difference in lactulose-to-mannitol ratio between larazotide acetate and placebo groups. Analysis showed that larazotide acetate resulted in a significant improvement in symptoms in the gluten challenge, but not in the gluten-free subjects. The larazotide acetate group reported a favorable change in celiac-disease gastrointestinal symptom rating scale (celiac disease-GSRS) in the gluten challenge patients, compared with the gluten-free patients. Compared to the placebo, larazotide acetate reduced incidents of "adverse event" (AE) gluten-related diarrhea in gluten challenge patients, while other AEs remained similar among the treatment groups. From their data, the study team concludes that larazotide acetate is well-tolerated in patients, and better than a placebo at relieving celiac-related gastrointestinal symptoms. This article has not been peer reviewed. It reports new, un-evaluated, medical research, and should not be used to guide clinical practice. Read more about using larazotide acetate to treat celiac disease at Merxiv.org.
- 6 comments
-
Celiac.com 05/20/2023 - This is the final chapter of Dr. Jean Duane's eBook, and we would like to thank Dr. Jean Duane for publishing Gluten-Centric Culture on Celiac.com. Gluten Centricity We live in a gluten-centric culture where severe dietary restrictions are associated with diminished social activities. Feeling excluded and observing that gluten was a punch line in nearly every form of media encountered, I wanted to research associations between given “truths” to illustrate how gluten centricity affects the lived experiences of those with celiac disease and/or food sensitivities (Chapter 1). I felt there was a lot more to the lifestyle than just figuring out “what’s for dinner!” Living the gluten-free lifestyle seemed to negatively affect nearly every social engagement I attended. I felt isolated when not able to participate in simple acts of commensality with family and friends. Considering current numbers of Americans with dietary restrictions, I determined that I could not be the only one feeling this way. In the process of writing this book, I read hundreds of studies focused on people living with food allergies (Duane, 2019). Most studies centered on children, few on adults, and fewer on the social impacts. This led me to developing a nation-wide study concentrating on food-sensitive adults living with other adults to attempt to fill the gap in the literature. Those of us with gluten sensitivities sometimes find ourselves at odds in social rituals, from taking communion in church to sharing the same foods around the dinner table (Chapter 3). We’re even omitted from the USDA food guidelines (Chapter 2). Our disease often isn’t taken as seriously as other diseases that revolve around eating a restrictive diet such as heart disease or diabetes. Furthermore, women report not being “heard” by doctors, extending the time until diagnosed (Chapter 4). We are often met with suspicion, accused of being faddish, or exaggerating our needs. We are subjected to a host of attitudes that reinforce this behavior and that cause us to feel like we are taking risks in our efforts to gracefully navigate life. It’s Actually Common Awareness of gluten sensitivity is growing. As we age, many reach the threshold of no-tolerance and experience an onset of chronic physical conditions. Some never associate their maladies with their diet, but those who do usually make adjustments. Gluten sensitivity spans all ages, classes, and races (Fasano & Catassi, 2012), making it unclear why American doctors do not lead with celiac disease tests, and why it takes patients an average of eleven years to get a diagnosis (Green & Jabri, 2003). Perhaps it is because celiac disease did not appear in the 1994 reports from either the U.S. Department of Health and Human Services or the National Institute of Diabetes and Digestive and Kidney Diseases (Fasano & Flaherty, 2014). Though it was known in Europe since 1941 (van Berge-Henegouwen & Mulder, 1993), until the early 2000s, U.S. doctors seemed to think that celiac disease bypassed North America (Fasano & Flaherty, 2014). Commenting on its growing ubiquity, Grain Brain authors declare, “Gluten is this generation’s tobacco” (Perlmutter & Loberg, 2013, p. 64) and one of the “greatest and most under-recognized health threats to humanity” (p. 32). Awareness by medical professionals provides hope to all people whose immune systems treat gluten as a “component of a dangerous bacterium or bacteria…toxic to humankind” (Fasano & Flaherty, 2014, Loc. 638). Certainly, the statistics are compelling; however, gluten-intolerance is still under-diagnosed. Let’s face it. It’s a hassle to be properly diagnosed and can be a burden to live with. But diagnosis doesn’t have to be a social “death sentence.” This book is an attempt to help with the social aspects of living with food sensitivities. Understanding is the first step. Previous chapters identify the cultural constraints that make us feel isolated and subjugated from mainstream culture (Chapter 1 and 2). Next, we examine “vexing venues” (Chapter 5) and ways we can take action to move from feeling excluded to being included. We see how we go through the Big (homeostatic) Shift, enabling us to have confidence in our lifestyle choices (Chapter 6 and 7). We now have empowering language so that we can conduct life gracefully (Chapter 8). Finally, we expect respect and compassion from others (Chapter 9). Another way to be empowered is to be aware of the laws in our country, such as understanding our rights under the American Disabilities Act, the subject of this chapter. Laws (are supposed to) Mandate Behavior Though this book does not dwell on the legal aspects of celiac disease, it is paramount to understand our rights to force compliance and to unite to expand the law’s definition. Visible disabilities such as impaired mobility or vision are covered under the American Disabilities Act, requiring accessibility in public pathways. Invisible disabilities such as diabetes, multiple sclerosis, lupus, and cystic fibrosis (ADA, 1990) carry the expectation that they will also be accommodated. Similarly, celiac disease and food allergies were added to the American Disabilities Act in 2012 with caveats when college students who felt their needs were not properly addressed, took action. Students with celiac disease and food sensitivities at Lesley University felt excluded and discriminated against because they were not able to fully enjoy the food service accommodations without fear of being cross-contaminated when purchasing the school’s mandatory meal plan. An ensuing lawsuit between Lesley University and the Justice Department determined that Lesley must provide gluten-free foods in its dining halls for students who have celiac disease or food allergies (Justice.gov). Further, celiac disease was deemed a disability under the American Disabilities Act (DOJ, 2012). The settlement also required Lesley to develop individualized meal plans, provide safe zones to prevent cross-contamination, disclose ingredients of foods, and pay $50,000 compensatory damages “to previously identified students who have celiac disease or other food allergies” (DOJ, 2012). Students attending this university now experience inclusiveness because several gluten-free selections are available in dining halls. The meals are prepared in a “clean” allergy-free space in the kitchen. Since the 2012 lawsuit, Lesley University has become a model of celiac disease inclusivity, providing a kitchen free of allergens, offering the foods requested by students, listening to students’ needs, training staff on safe handling, and cross-contamination practices (Schilling, 2015). This landmark case influenced the outcome of a similar suit against Rider University in 2019 where students with similar complaints as those attending Lesley were rewarded with inclusive accommodations on campus (DOJ, 2019). ADA and the School Venue The American Disabilities Act does not detail specific residency standards, however Title II states that “no qualified individual with a disability shall, by reason of such disability, be excluded from participation in or be denied the benefits of the services, programs, or activities of a public entity, or be subjected to discrimination by any such entity (ADA, 2012).” This means that if a student attends a school that receives federal funding (and most do), they are entitled to the rights stated in the American Disabilities Act. But because it is vaguely written, some institutions offer gluten-free dorm rooms, while others require celiac disease students to live in an apartment off campus. Sarah (#31) describes how the school’s staff met with her to figure out a solution (Chapter 3). Though intended to protect her from cross-contamination, the ensuing plan caused her to experience a lonely first year in the school venue because she was forbidden from entering dining halls and other food-events such as college pizza parties. She suffered extreme isolation that prevented her from bonding with her fellow students. When universities require students living on campus to purchase a meal plan, it can create a burden for students trying to eat safely. For example, student and celiac disease sufferer Hannah Smith ( Smith v. University of Maryland, 2020) was forced to purchase a meal plan and alleges that her university served her gluten-containing food three times, despite asking whether it was gluten free. On one occasion, a campus staff member “berated Smith and served her blackened toast for making a complaint” (AP, 2/24/20). On another occasion, Smith was assured that a popular breakfast cereal containing wheat was gluten free ( Smith v. University of Maryland, 2020) and then for lunch, served her soup that contained barley. The university refused to refund her for the cost of her meal plan when she moved off campus the next year, so she sued. In the heartbreaking complaint prepared by Smith’s lawyer, it says the honor student after consuming the food, “vomited so intensely that blood vessels throughout her face burst. She experienced brain fog, difficulty walking, uncontrollable vomiting, and rib pain as a result of projectile vomiting. The impact of this incident lasted for weeks.” Over the course of the semester, she developed dermatitis herpetiformis. Further it says, because of these incidents, “she could not maintain her grades due to constant illness” caused from becoming sickened by the gluten-containing foods. Finally, it summarized, “Smith suffered physical, emotional, and financial harm as a result of the Defendant’s conduct” ( Smith v. University of Maryland, 2020). Ultimately, the suit was dropped. The position of the school in this situation enacted the I-know-best, gluten-doubt, and the able-body biases , despite Smith’s father’s attempt to educate and ensure his daughter had safe fare. The kitchen staff did not ever seem to embrace Smith’s serious requirements with their actions of repeatedly exposing her to gluten (while assuring her the foods were safe). This lawsuit very disturbing because the repeated efforts of Smith’s father did not yield success. It implies that we are truly at the mercy of the willingness of those in charge when we are in any kind of institution or situation where we have to rely on others to feed us. Flexible guidelines in the American Disabilities Act allow colleges to work with what they have in order to accommodate student’s needs. Sometimes arrangements instill inclusive behavior, and other times they result in unintended consequences such as isolating a student, or dependence on non-compliant kitchen staff. It comes down to training everyone involved and being dedicated to working together to accomplish the goal of providing a safe meal to the student. When the Lesley case mandated that celiac disease and food allergies were included in the American Disabilities Act, it was hoped that there would be a ripple effect to make it safer for our community to dine in restaurants. Though it has improved some situations, the American Disabilities Act contains exceptions for restaurants. American Disabilities Act and Restaurants Nearly every participant commented on how they were afraid to eat out because of inconsistencies in compliance. Not feeling safe to eat restaurant food was by far the reason many felt isolated and excluded from social gatherings because of their disease. Chapter 9 details strategies for restaurant eating. Here, let’s look at the laws about celiac disease as a disability. The American Disabilities Act falls short when it comes to restaurants, because if a patron’s request “alters the nature of the goods” the restaurant does not need to comply (ADA, 2012). This means the amended American Disabilities Act does not apply in the same way to restaurants as it does to institutions. Assuming you are properly diagnosed, you can demand a gluten-free meal at federally-funded institution but you have fewer legal rights in a restaurant. Restaurants can answer questions about ingredients and omit or substitute according to a patron’s request but they do not need to provide “different foods to meet particular dietary needs” (ADA, 2012). As we have heard from participants, this causes every restaurant experience to be unique, depending on the commitment level and knowledge of the staff. If restaurants do not want to “alter the nature of their goods” to comply with gluten free guidelines, they can refuse to serve those with celiac disease and food sensitivities (U.S. Fed News, 2012). Consequently, this continues to make restaurants a “vexing venue” because they are still not required to offer safe gluten free meals. Some restaurants have conscientious staff, but others do not. Furthermore, a restaurant that is compliant one day may not be the next because standards vary by state, by restaurant, and by servers and chefs. The Gluten Intolerance Group of North America’s Gluten-Free Food Service program provides food service providers with guidelines to be designated as a Gluten Free Safe Spot (gffs.org). This kind of training throughout the restaurant industry would ensure consistency. This website also provides information on restaurants, schools, hospitals and senior facilities who have attained the Gluten Free Safe Spot designation. Trusting the server and the restaurant to comply is often an act of faith. Just as when we travel to another country, we represent all Americans, when we ask for a special meal in a restaurant, we are “representing” all of those who have celiac disease or food sensitivities. When restaurants get it “right,” participants describe how they praise the staff, often calling over the manager to thank them for accommodating our needs. Positively reinforcing good behavior might help the next person who asks for a special meal. But sometimes that backfires. Liza (#68) reported an incident when she asked the waiter for a gluten free, dairy free selection and the waiter said, “Not another special need! You should have heard how the lady at that table over there ordered. She even had a card with all of her requirements on it for me to give to the chef.” The waiter did not provide Liza with a meal she felt safe eating. She did not feel he listened to her needs because the salmon she ordered cooked “dry” came with some kind of brown sauce she was afraid to eat. Participants voiced they are careful not to appear too “demanding.” It is a slippery slope because we have to trust others to believe our needs and if we are “glutened,” we pay the price of being ill. Those with celiac disease who have been sickened from eating in restaurants previously may be less apt to trust establishments that promise gluten free selections. This was the case involving a boy who had celiac disease and who brought his own food on a school field trip to Colonial Williamsburg. He and his 60 classmates were planning to be entertained in the18th century style in a restaurant (Marimow, 2019). When it came time for the meal, the boy was told that the museum restaurant had a “no outside food” policy and said the he would need to eat the food prepared there. The father explained that on other occasions, the boy had been “glutened” in restaurants, which is why he brought his own food. The restaurant stood its ground and the boy and his father ate outside in the rain, away from his classmates. The father sued for discrimination under the American Disabilities Act (Hackman, 2017). The restaurant claimed that they offered the boy a gluten free meal and did not require him to leave, and that consuming “outside food” in their restaurant violated health regulations (AP Press, 5/31/19). A court found that the restaurant had previously made exceptions to the “no outside” rule, and because the child needed a safe meal, bringing his own food was considered “reasonable.” Further, his request “did not alter the nature of the restaurant’s services” (Boyns, 2020). A federal appeals court found in favor of the lad. State health departments often do not allow food brought from home by patrons to be heated up in restaurant kitchens because the restaurant assumes liability if they handle outside food. If you elect to bring your own food to a restaurant, ensure that it does not require special handling and refrain from asking the restaurant staff to handle it. Consider carrying a letter from your doctor stating you require a special diet (Chapter 9). Restaurant policies and state policies on outside food vary. It is a tricky business. While we want to show gratitude for restaurants that are avoiding able-bodied bias by offering gluten free and food sensitive selections, we are also relying on individuals who may not fully understand the plethora of ingredients that indicate gluten. For example, Todd Serlin became sickened from consuming French onion soup at a restaurant at the Grand Canyon in 2019 after being assured several times that it was gluten free (AP Press, 4/2/19) illustrating the I-know-best attitude on the part of the restaurant personnel. Another lawsuit claimed that those with celiac disease experience discrimination when a restaurant charged $1 more for gluten free provisions, and didn’t charge for peanut free or vegan requests (Hackman, 2017). We appreciate restaurant’s efforts, but often when we disclose we have celiac disease, we are sometimes warned not to consume the gluten free foods. For example, several pizza chains offer gluten free crust options, but issue the caveat that even though they take precautions, foods may be cross-contaminated because they do not have a strictly gluten free environment. It comes down to liability. I used to frequent a Mexican restaurant where I could get a salad and a piece of grilled fish. One day, when I ordered my normal fare, the manager came back to my table and presented me with a laminated disclaimer. It said, “We are not liable for your food allergies. If you consent to eat the foods we prepare for you, and you become sickened as a result, we relinquish all liability.” What a way to start a meal! First of all, I was the only one at the table that got the laminated disclaimer, so I felt embarrassed as my companions inquired about it. Also, I really didn’t want to risk eating anything there after they presented me with “legalese” to let them off the hook. I want to be reassured, not disclaimed. When my food came, I didn’t enjoy it. It was my last meal there. Can they just disclaim their liability like that? If the restaurant in the Grand Canyon present Serlin with a similar card, would he have had a claim against them when sickened? According to Craig, restaurants assume liability when consenting to provide a gluten free meal, causing some to take out insurance policies in case of slip-ups (Craig, 2012). Does the disclaimer create a loophole in the law? Restaurants continue to be a challenge for us because there are no standardized guidelines mandated by the government for them to follow. Until the American Disabilities Act removes the caveats, every restaurant outing poses risk for those of us with celiac disease or food sensitivities. Jean’s Story – A Restaurant in Dallas Dear Reader, I wish you could have been there with me to share this delightful meal! About ten years after being diagnosed and completely gluten free, the Lone Star Gluten Intolerance Group of North America asked me to speak at one of their meetings. They were so nice! Kay welcomed me into her home with open arms. I spent the night in her home and the next day she drove me to the venue where the group was meeting to hear my speech. After the speech, several group members took me to eat in a gluten-free restaurant. Everything on the menu was safe to eat. I don’t think that restaurant even used dairy products. I looked at the menu and instead of figuring out how I could get a salad with nothing on it to pick at, I looked at all of the selections with the knowledge that I could actually indulge in the meatloaf with mashed potatoes, the chicken fried steak with okra, or the Rueben sandwich. It was positively heavenly! It reminded me of the early part of my life when eating out was a daily activity. Back then my coworkers and I would plan our elaborate lunch schedule around various restaurant offerings. But after being diagnosed, I only went to restaurants to be sociable, often not even eating the salad, but rather cutting it up and pushing it around my plate. But at this glorious restaurant, I ordered fish and chips with coleslaw and gorged myself on that heavenly food. Oh, the crunchy batter on that light, white fish. Mmmm the crisp French fries and the amazing taste combinations when paired with the catsup and apple cider vinegar. The others around the table were indulging in other oral delights. They explained that this special restaurant was one place where they all felt safe and they ate there every Saturday at lunch. The cleaned plates were cleared and the waitress asked us what we would like for dessert. Dessert! Wow! I only ever have berries nowadays. What a treat! I ordered a lovely lemon cake with lemony icing. It was one of the most wonderful meals I can remember eating. I want to live in a world where I can order from menus like that again! Thank you to the Lone Star Gluten Intolerance Group for giving me such a fond memory, and especially thank you to that restaurant. (Sadly, that fine restaurant is no longer in business.) Let’s work together, so we can all eat in restaurants without worry again! American Disabilities Act and Institutions The inclusion of celiac disease in the American Disabilities Act as a result of the 2012 lawsuit requires institutions like colleges, hospitals, prisons, and universities to comply when meals are prepared “in house.” For institutions, the ruling mandates that those with food allergies, non-celiac gluten sensitivity, and celiac disease can provide grocery lists to food providers who must be trained on safe practices. It mandates that allergen-free meals can be pre-ordered; and that those with celiac disease or food sensitivities will be provided a designated area to eat and to store their food. However, private institutions such as elder care facilities are not required to comply (Chapter 2). Title III of the American Disabilities Act does not allow employers to discriminate against, or not hire, a person with celiac disease if they are otherwise qualified. It requires that employers who offer meals to employees provide gluten free alternatives for those with celiac disease or food sensitivities. It states that emergency services such as safe shelters or institutions such as jails must offer gluten free meals, and it allows a person with celiac disease to bring foods into places serving foods that are not safe. There are several delivery services that cater to various food allergies (Healthline, 2023). The American Disabilities Act does not require hospitals to provide gluten free pharmaceuticals. I had the misfortunate of being involved in a hit-and-run on the highway. I was taken to the hospital in an ambulance and was in considerable pain. My sternum was cracked. The staff at the hospital could not give me pain medication because they could not guarantee me that it was gluten free. It took me an entire miserable day to track down safe medicine (using the Internet and coordinating with my doctor). This was a terrible experience, and one that simply has to change. The celiac.org organization works to present legislation for things like this. The change to the American Disabilities Act to include celiac disease is a positive move, but it needs to be broadened to include all public places, restaurants, pharmaceuticals, etc. modeling how those who are physically disabled are accommodated. Here are some proposed amendments to the American Disabilities Act we could suggest to our Congress representative, which would go a long way toward expanding our accessibility: Restaurants would be required to list the ingredients of every dish, either on the menu, or by request. (That would help those with food sensitivities to determine for themselves what is safe, rather than relying on everyone they ask to know all of the many ingredient names that can mean gluten, dairy, or other allergens.) Restaurants would be required to follow the safe-practices guidelines provided by an organization such as the Gluten Intolerance Group of North America (gluten.org / gffs.org) to eliminate cross-contamination, and to properly train restaurant staff. Furthermore, they would be required to publicly post their safe-practices certification in a place visible to patrons. Restaurants would be required to offer several pre-cooked, frozen meal options prepared in an offsite, gluten free certified “safe” kitchen that would just require heating (in the packaging to prevent cross-contamination). That pre-cooked meal wouldn’t require any alterations or substitutions in the regular fare a restaurant offers, but it would ensure that everyone with celiac disease or food sensitivities would have something they knew they could eat. (This may not be optimal, but at least those with celiac disease would be assured of something to order when they go out.) Pharmaceutical companies would be required to prominently disclose all ingredients on the outside label (in plain English, not in medical terminology) and which known allergens the product contains. Ingredients would be specified in each lot, so rather than saying “starch,” label the exact starch used (corn, potato, wheat, rice, etc.). Food manufacturers would write ingredient labels in plain English. For example, if the ingredient is “maltodextrin,” the label would be required to say whether it was derived from corn, rice, potato starch, or wheat. American Disabilities Act and Other Disabilities The National Institutes of Health estimate that there are approximately 3.2 million visually impaired Americans (NIH, 2018). Americans over the age of 15 in a wheelchair number 3.6 million (U.S. Census, 2012). The American gluten-sensitive population sums 20 million conservatively (Fasano and Catassi, 2012; Fasano et al., 2015), including three million people with celiac disease (Fasano et al., 2003) and three million with non-celiac gluten sensitivity (Uhde et al., 2016). In fact, those suffering with gluten sensitivities outnumber individuals who are visually impaired or in a wheelchair combined; yet, the model used to accommodate the visually and mobility impaired has not been extended to those of us with celiac disease or food sensitivities. If laws were changed to require accessibility to accommodate the needs of those with gluten sensitivities such as amending the American Disabilities Act; similar to the “bubbles” installed at crosswalks across the country for the vision impaired, swimming pool lifts, and ramps in public buildings for individuals in wheelchairs, those with celiac disease would be able to safely navigate aspects of life. Taking Action A peaceful organized effort may bring attention to our need to be accommodated. This starts with unification, via gluten-oriented organizations, social media, or community activities to gain nation-wide awareness. It requires that we use similar language such as the ideologies and cultural constraints defined in this book, uniformity in how we communicate our requests in public places, and advocating education, respect, and compassion in our daily lives. Just as those in wheelchairs can cross streets and access public buildings, it is my hope that this work can influence positive change in the celiac community. Followers of the gluten free diet band together, perpetuating their beliefs that they can cultivate a healthy body and rid themselves from disease through diet. Organizations form to educate and change laws. United, devoted dietary followers create massive awareness. In the same way that other peaceful demonstrations have brought attention to the oppression of others, perhaps a campaign that develops the notion being aware of #glutencentric introduced in the last chapter would bring light to our plight, and possibly affect positive changes. We now have a hashtag to “call out” those in the media who ridicule our disease. Just as we may incorporate the catch phrase such as #glutencentric to signify our gluten free lifestyle, we may also develop a catch phrase to bring attention to celebrities who use gluten as the butt of jokes. How about #glutenbutthead? Perhaps doing this on social media would affect a positive change in the global attitudes. It seems ridiculous that we’d have to do this. People with other diseases don’t have catch phrases to be taken seriously, but it seems we need one since “gluten” mocking is consistent in TV scripts, in newspapers, and a subject for comedians. Next, I want to talk about a final cultural constraint that revealed itself in my study. Even though I gave you a sneak peek in Chapter 8’s summary, I saved this one for this final chapter because it has a happy ending (with some hopeful diagnostic tests on the horizon). Many participants observe that family members have symptoms they associate with celiac disease, and when they encouraged them to seek medical help, they refused. This was described so frequently that I determined there is another cultural constraint prompting this behavior. It’s the yours, not mine stance. Yours, Not Mine Stance We mean well when we suggest it may be gluten causing the problems for our loved ones. After all, celiac disease is a genetic disease, so it makes sense that relatives are tested when a family member is diagnosed. However, there is a phenomenon I have observed from analyzing the interview data when family members resist seeking a medical opinion. Recall the lady I met in the pet shop who described her niece’s diet (Chapter 1). When I asked her if the family was following it, she said, “None of us are going to follow that diet.” Considering that her niece was diagnosed with celiac disease, there is a strong likelihood that someone else in that family had it too – and should be following the diet. But that family elected to make the niece feel like the odd one out. This is an example of the yours, not mine stance where family members treat celiac disease as “your” disease, not “mine.” Some people in my study report cooperative family situations where everyone “embraced” the gluten free diet and worked together to help the member with celiac disease. But many describe how immediate and extended family members treated them like it was something unique to the diagnosed individual—not something they could also have. This caused personal strife, as well as a reluctance to recommend that symptomatic family members get tested. When people first hear of something they fear, one coping mechanism is to protect themselves by separating from and even denying the situation (Manoogian, Harter, & Denham, 2010). It is human nature and a primal survival tactic. Understanding the yours, not mine response as a normal knee-jerk reaction helps us to comprehend why family reacts the way they do when we are trying to be helpful. This poses the question: How do we help our family members who have symptoms we attribute to gluten consumption? The first step is to understand the tendency toward the yours, not mine mentality. William (#30) says, “We can spot them,” referring to how those diagnosed with celiac disease can see the symptoms in other family members. Those of us who live with the disease, and who are well informed about the many manifestations of gluten intolerance “just know” that other family members may be reacting to gluten. We hear our family complain of indications ranging from joint pain, migraines, swelling, brain-fog, gas, bloating, back pain, leg numbness, rosacea on the nose, and gastro-intestinal issues (Fasano & Flaherty, 2014), to name a few. When we mention it might be gluten causing the problems, the response is often, “It can’t be, I’ve eaten it all my life!” When people say that, I want to say, “I rest my case!” It is fascinating how food operates in multiple dimensions of life. In the case of the individual, in the “body battleground,” (Chapter 4) food choices cause harmony for those who are aware of what makes their body thrive, or havoc for those who don’t. Like many interviewed who associate their physical maladies with what they eat, I see it on other people. It presents a constant dilemma for me to decide whether to say something, or to keep my big mouth shut. Usually, I say something and wish afterward that I didn’t. Nobody wants to be told your “truth” even if you’ve spent decades learning it, and suffered for years in the process. Their attitudes, in general are: yours, not mine . We don’t want our boats to be rocked. We want to eat whatever we want, with no consequences. It takes time to come to terms with a restrictive diet. There are actually over 200 symptoms of gluten intolerance (Wangen, 2009, p. 37). For example, Dustin (#46) reports, “My teeth started falling apart. They had cracks and cavities. The dentist said they were ‘demineralizing.’” Vivian (#51) says, “I had low bone density and lots of fillings in my teeth.” Cara (#53) says, “I had a lot of problems with my teeth, brain fog, joint pain, headaches, migraines, kidney problems, skin rashes, and hair loss.” We also know how positively the body responds to a gluten free diet and often want to share our knowledge and secret to thriving health with our family members. What kind of kinfolk would we be if we didn’t? On the other hand, we don’t want to become “that person” who attributes every malady to gluten, though scientific studies exist to support that premise. For example, remember Emery (#45) when she observed symptoms of gout in her uncle and inflammation in her nephews. While at a family dinner, she reminded them “her celiac disease” is a genetic disorder, and was met with the response, “What? Aren’t you just being dramatic? Maybe you are following the diet to get attention (Chapter 5)?” As mentioned before, that illustrates gluten-doubt , but it also shows the yours, not mine mentality found in many families. Other respondents said family members object to eliminating wheat from the diet for religious purposes, citing the Bible sanctifying wheat for human consumption (see Psalms 81:16; Psalms 147:14; Ezekiel 4:9; Joel 2:24). By incorporating the yours, not mine stance family members can erect a shield to protect themselves or loved ones from facing the inconveniences associated with celiac disease. Recall Ava’s (#7) daughter who exhibits symptoms of celiac disease, but refuses to be tested because she (erroneously) believes it “skips a generation” (Chapter 5). This is a convenient yours, not mine adaptation that keeps the mother’s disease compartmentalized as “hers” and not “ours.” However, when family members embrace our disease, we have a better chance of surviving. People suffering heart problems tended to survive longer when spouses referred to the problem as “ours” versus “yours” (Rohrbaugh, et al., 2000, p. 781). People with a disease who live in families who accept the it as “ours” are much more likely to succeed. Successfully “coping with stressful life circumstances is a social process” (Lyons, et al., 1998, p. 582). However, the phenomenon of yours, not mine seems to be an initial response while inclusiveness evolves over time with familial acceptance. With a compassionate understanding that the yours, not mine attitude is often an initial survival tactic, we may eventually be able to gently urge loved ones to get tests that may ultimately save their lives. Let’s be clear: we’re not trying to give medical advice. We are just offering our hard-earned knowledge to urge symptomatic family members go to a bona fide doctor to get tested. Though, as we know, it may send them down a difficult path because as many respondents reported, they were initially misdiagnosed. Hope on the Horizon A study conducted by (Megiorni, et al., 2008) found that 90% of European white patients carry the genetic markers for celiac disease, meaning they may develop it sometime in their lifetime. They also found that females are twice as likely to develop it than males (p. 997). Assuming family members eventually come around, to want to understand the cause of their symptoms, what do we say? We may suggest they go to their doctor for some “tests,” but considering that many doctors are misinformed about celiac disease, they may be sent away with “negative results.” Many doctors still believe celiac disease is rare, but because of the work of luminaries such as Dr. Alessio Fasano, Dr. Peter Green and others, we now know that gluten intolerance is fairly common, and that customary serologic testing may not be conclusive. Therefore, accurate outcomes rely on what doctor is chosen and what tests the doctor chooses to prescribe to obtain a diagnosis. Inconsistencies in the diagnosis process contributes to the yours, not mine effect because family members may undergo what they think is comprehensive testing, but may not have been properly assessed. For those who recognize their symptoms may be associated with gluten and who earnestly want to seek a proper diagnosis, there are several tests that are emerging beyond the endoscopy and serological routines. Stool tests and several home tests available now to test whether you have the genetic (HLA) marker, or if you have the antibodies. This is significant because many who have the traditional “celiac panel” blood tests, test negative for the disease (Celiac.org), possibly because the disease has not progressed enough to appear as antibodies in the blood. Other tests are now available for early detection such as a fingertip blood test has been developed to screen first-degree relatives for celiac disease as a first pass (Popp, et al., 2013). It tests for IgA class and EMA antibodies. An HLA-DQ gene marker test (a cheek swab) can determine with 90% accuracy whether someone has a pre-disposition to develop celiac disease (Tollefsen, et al., 2006). Our community had high hopes for the drug called larazotide (also known as INN-202 and AT-1001) studied on those with celiac disease (CDF, 2019). However, the trials ended in Phase 3 (9 Meters, 2022; CDF, 2019). Another treatment researched uses bifidobacterium probiotics to assist the body to “break down gluten and potentially tame the body’s immune system” (Klemenak, 2015). Between new diagnostic procedures and pharmaceutical developments, there is hope! These early testing methods are exciting developments for family members who may have tested negative to customary tests, but who still exhibit symptoms. Medical diagnostic inconsistencies contribute to the yours, not mine and gluten-doubt attitudes. If we felt our family members were correctly tested, we would be more at ease with a negative diagnosis, but unfortunately because of testing inconsistencies, there is often doubt about whether a family member was properly tested, even after seeking medical input. Summary The purpose of this work is to validate the voices of people living with celiac disease and non-celiac gluten sensitivity to create an awareness of the cultural constraints that influence thinking about gluten sensitivities. Additional outcomes include offering best practices to enhance social interactions for this community and broadening the current definition of celiac disease accessibility in the American Disabilities Act. Scholars have considered the cultural aspects of food and studied the effect of hidden disabilities on quality of life. However, few have synthesized the impact of living with food allergies on cultural and social aspects of everyday life. The degree of ease with which those diagnosed with celiac disease navigate life seems dependent on how reactive their bodies are. Those who are asymptomatic can blend into the crowd, take a few risks and eat gluten free meals at restaurants. Contrastingly, those who are highly sensitive often do not go out at all, and if they do, they bring their own food, or ask a lot of questions before consuming foods. In the other venues, we see similar attitudes where long-held “truths” remain intransigent. Our new awareness of the cultural constraints presented in this book, along with the venues where these attitudes are constantly challenged empowers us. Now we have language and tools in our lexicon to broach a discussion to bring about a different awareness. Even if we don’t have a conversation, it helps us to have a way of thinking about it so we don’t feel victimized, isolated, or at the mercy of others to ensure our health and safety. Moving forward, our newfound knowledge, willingness to advocate our needs, and determination can positively transform our lives. Jean’s Redemption After I was diagnosed and began to research celiac disease, I realized that the constant stomachache that made me fear pregnancy and that my previous abnormal pregnancies were likely caused from the undiagnosed disease. Just as inappropriate food choices may have contributed to my father’s early death, consuming gluten all those years before being diagnosed cost my husband and myself a family. In parts of Europe, children are assessed for celiac disease between the ages two and four years old (Popp, A., & Maki, M., 2019). Here in the USA, we’re lucky to be diagnosed by middle age, and often misdiagnosed prior to an accurate diagnosis. If I had been diagnosed when I was younger, I would have been rid of the symptoms, free of pain, and probably had a body that could have endured a pregnancy. Life may have turned out completely different for my husband and me. But my story is one of redemption and transformation. By eliminating the foods that are poison to my body, I thrive and remain grateful for what I have, living an alternative path. It led me to start a company called Alternative Cook, LLC (alternativecook.com), to produce instructional video streams, cookbooks, courses, and consulting. Through all this, I realized that celiac disease is a social issue. My passion for this cause led me to pursue a PhD and carry out the study and write this book. It is my sincere hope that I can have a positive influence on those who live with this disease. Discussion Questions: What amendments would you propose to the American Disabilities Act to enhance our restaurant experience? How can we unite to change the American Disabilities Act to ensure we can go out to eat safely in any restaurant we desire to patronize? What examples can you provide of the yours, not mine stance? References in Chapter 10 9Meters. (2022). 9Meters discontinues phase 3 clinical trial for potential celiac disease drug larazotide. Retrieved 7/1/22 from https://celiac.org/about-the-foundation/featured-news/2022/06/9-meters-discontinues-phase-3-clinical-trial-for-potential-celiac-disease-drug-larazotide/ American Disabilities Act Title III Assistance Manual. Retrieved from https://www.ada.gov/taman3.htm American Disabilities Act. (1990). Retrieved from https://www.ada.gov/ American Disabilities Act. (2012). Questions and answers about the Lesley University agreement and potential implications for individuals with food allergies. Department of Justice. Retrieved from https://www.ada.gov/q&a_lesley_university.htm AP Press. (5/31/19). Court: Lawsuit over boy's gluten-free meal can proceed; Court: Lawsuit over boy's gluten-free meal can proceed. Canadian Press. Retrieved from https://advance-lexis-com.du.idm.oclc.org/api/document?collection=news&id=urn:contentItem:5W7N-CMW1-DY9S-T3Y3-00000-00&context=1516831. AP Press. (April 2, 2019 Tuesday). Man sickened after eating gluten at Grand Canyon hotel sues; Man sickened after eating gluten at Grand Canyon hotel sues. Canadian Press. Retrieved from https://advance-lexis-com.du.idm.oclc.org/api/document?collection=news&id=urn:contentItem:5VT4-C2S1-DY9S-T1HK-00000-00&context=1516831. Boyns, S. (January 10, 2020 Friday). Workplace Law; Is gluten sensitivity considered a disability? Monterey County Herald (California). Retrieved from https://advance-lexis-com.du.idm.oclc.org/api/document?collection=news&id=urn:contentItem:5XY7-DF61-JBCN-43VV-00000-00&context=1516831 Celiac Disease Foundation. Retrieved from https://celiac.org/ Celiac Disease Foundation. (2019). First patient dosed in first ever phase 3 clinical trial for celiac disease. Retrieved from https://celiac.org/about-the-foundation/featured-news/2019/08/first-patient-dosed-in-first-ever-phase-3-clinical-trial-for-celiac-disease/ Craig, B. (September 18, 2012). Protect yourself as well as your customers; Companies that offer restaurant liability insurance have begun expanding policies to cover claims related to gluten reactions as well as food poisoning and allergic reactions.. QSRweb. Retrieved from https://advance-lexis-com.du.idm.oclc.org/api/document?collection=news&id=urn:contentItem:57VC-9X01-DXN1-20Y3-00000-00&context=1516831. DOJ. (2012). Justice department and Lesley University sign agreement to ensure meal plan is inclusive of students with celiac disease and food allergies. Retrieved November 18, 2018 from https://www.justice.gov/opa/pr/justice-department-and-lesley-university-sign-agreement-ensure-meal-plan-inclusive-students DOJ. (2019). U.S. attorney’s office reaches agreement with Rider University to resolve allegations under the American with Disabilities Act. Retrieved from https://www.justice.gov/usao-nj/pr/us-attorney-s-office-reaches-agreement-rider-university-resolve-allegations-under Duane, J. (2019) Social aspects of food sensitivities. Retrieved from https://digitalcommons.du.edu/etd/1573/ Fasano, A., & Catassi, C. (2012). Celiac disease. The New England Journal of Medicine, 267 (25), 2419-2426. doi: 10.1056/NEJMcp1113994 Fasano, A., & Flaherty. S. (2014). Gluten freedom . Hoboken, NJ: Wiley & Sons Inc. Fasano, A., Berti, I., Gerarduzzi, T., Not, T., Colletti, R., Drago, S., Elitsur, Y., Green, P., Guandalini. S., Hill, I., Pietzak, M., Ventura, A., Thorpe, M., Kryszak, D., Fornaroli, F., Wasserman, S., Murray, J., & Horvath, M. (2003). Prevalence of celiac disease in at-risk and not-at-risk groups in the United States. Arch Intern Med, 163 , 286-292. doi: 10.1001/archinte.163.3.286 Fasano, A., Sapone, A., Zevallos, V., & Schuppan, D. (2015). Nonceliac gluten and wheat sensitivity. Gastroenterology, 148 , 1195-1204. doi: 10.1053/j.gastro.2014.12049 Green, P. H. R., & Jabri, B. (2003). Coeliac disease. The Lancet 362 , 383-391. doi: 10.1016/S0140-6736(03)14027-5 Hackman, L. (2017). Franchise litigation rising over dietary considerations . Newstext, LLC. Retrieved from https://advance-lexis-com.du.idm.oclc.org/api/document?collection=news&id=urn:contentItem:5PDH-58D1-JCMN-Y51F-00000-00&context=1516831. Healthline. GF Food Delivery Services. Retrieved from https://www.healthline.com/nutrition/gluten-free-meal-delivery Klemenak, M., Dolinsek, J., Langerholc, Tomaz, Di Gioia, D., Micetic-Turk, D. (2015). Administration of Bifidobacterium breve decreases the production of TNF-a in children with celiac disease. Digestive Diseases and Sciences 60 (11), 3386-3392. doi: 10.1007/s10620-015-3769-7 Lyons, R., Mickelson, K., Sullivan, M., & Coyne, J. (1998). Coping as a communal process. Journal of Social and Personal Relationships, 15 (5), 579-605. No doi. Manoogian, M. M., Harter, L. M., & Denham, S. A. (2013). Storied nature of health legacies in the familial experience of type 2 diabetes. In J. Koenig Kellas (Ed.), Family Storytelling: Negotiating Identities, Teaching Lessons, and Making Meaning (pp. 79-96). New York, NY: Routledge. Marimow, A. (2019) A boy, a chicken sandwich and a federal case over dinner at Colonial Williamsburg. Retrieved from https://www.washingtonpost.com/local/legal-issues/a-boy-a-chicken-sandwich-and-a-federal-case-over-dinner-at-colonial-williamsburg/2019/05/31/4fc7763c-83d6-11e9-95a9-e2c830afe24f_story.html Megiorni, F., Mora, B., Bonomico, M., Barbato, M., Montuori, M. Viola, F., Trabace, S., & Mazzilli, M. (2008). HLA-DQ and susceptibility to celiac disease: Evidence for gender differences and parent-of-origin effects. American Journal of Gastroenterology . doi: 10.111/j.1572-0241.2007.01716.x NIH. (2018). Visual impairment, blindness cases in U.S. expected to double by 2050. National Institutes of health. Retrieved November 20, 2018 from https://www.nih.gov/news-events/news-releases/visual-impairment-blindness-cases-us-expected-double-2050 Perlmutter, D., & Loberg, K. (2013). Grain brain: The surprising truth about wheat, carbs, and sugar – your brain’s silent killers . Little Brown and Company: New York, NY. Popp, A., Jinga, M., Jurcut, C., Balaban, V., Bardas, C., Laurila, K., Vasilescu, F., Ene., A., Anca., I., & Mäki, M. (2013). Fingertip rapid point-of-care test in adult case-finding in coeliac disease. Gastroenterology, 13 (115). http://www.biomedcentral.com/1471-230X/13/115 Popp, A., & Mäki, M. (2019). Changing pattern of childhood celiac disease epidemiology: contributing factors. Front Pediatrics, 7(357). doi: 10.3389/fped.2019.00357 Rohrbaugh, M. J., Mehl, M. R., Shoham, V., Reilly, E. S., & Ewy, G. A. (2008). Prognostic significance of spouse we talk in couples coping with heart failure. Journal of Consulting and Clinical Psychology, 76 (5), 781-789. doi: 10.1037/0893-3200.16.1.3 Schilling, B. (2015). Lesley U after the food allergy Justice settlement. Food Management (Penton). Retrieved from https://advance-lexis-com.du.idm.oclc.org/api/document?collection=news&id=urn:contentItem:5GMH-Y6J1-DY2W-F4G4-00000-00&context=1516831. Smith v University of Maryland. (2020). Case 8:20-cv-00433-TDC. Filed 2/20/20. Retrieved from https://www.courtlistener.com/docket/16868125/smith-v-university-of-maryland-college-park/ AP Press (2020). Suit: University fed gluten to student with celiac disease . College Park, MD. Retrieved from Nexis-Lexis May 5, 2020. https://advance-lexis-com.du.idm.oclc.org/document/?pdmfid=1516831&crid=469f1327-8692-4a7a-9b24-bf52c26bbccf&pddocfullpath=%2Fshared%2Fdocument%2Fnews%2Furn%3AcontentItem%3A5Y90-8D21-JC65-52YB-00000-00&pdcontentcomponentid=304481&pdteaserkey=sr0&pditab=allpods&ecomp=-763k&earg=sr0&prid=77a0f70b-607a-4db6-a39d-30f293c477fd Tollefsen, S., Arentz-Hansen, H., Fleckenstein, B., Molberg, O., Raki, M., Kwok, W., Gunther, J., Lundin, K., & Sollid, L., (2006). HLA-DQ2 and –DQ8 signatures of gluten T cell epitopes in celiac disease. Journal of Clinical Investigation, 116 (8). doi: 10.1172/JC127620 U.S. Census. (2012). Nearly 1 in 5 people have a disability in the U.S . Retrieved November 10, 2018 from https://www.census.gov/newsroom/releases/archives/miscellaneous/cb12-134.html U.S. Fed News (2012). Justice Department And Lesley University Sign Agreement To Ensure Meal Plan Is Inclusive Of Students With Celiac Disease And Food Allergies. U.S. Fed News. Retrieved from https://advance-lexis-com.du.idm.oclc.org/api/document?collection=news&id=urn:contentItem:57B4-BC11-F12F-F356-00000-00&context=1516831. Uhde, M., Ajamian, M., Caio. G., DeGiorgio, R., Indart, A., Green, P., Verna, E. Volta, U., & Alaedini, A. (2016). Intestinal cell damage and systemic immune activation in individuals reporting sensitivity to wheat in the absence of coeliac disease. Gut, 65 , 1930-1937. doi: 10.1136/gutjrl-2016-211964 van Berge-Henegouwen & Mulder (1993). Pioneer in the gluten free diet: Willem-Karel Dicke 1905-1962, over 50 years of gluten free diet. Gut, 34, 1473-1475. doi: 10.1136/gut.34/11/1473 Wangen, S. (2009). Healthier without wheat . Seattle, WA: Innate Health Publishing. Copyright © 2021 by Alternative Cook, LLC All rights reserved. Published in the United States by Alternative Cook, LLC LIBRARY OF CONGRESS CATALOGING-IN-PUBLICATION Data Names: Duane, Jean Elizabeth, PhD, Author. Title: Gluten-Centric Culture, A Commensality Conundrum Description: Centennial, CO: Alternative Cook, LLC, 2021 Identifiers: ISBN 978-0-9787109-2-7 (hardcover) ISBN 978-0-9787109-3-4 (ebook) Subjects: Social Science, Food Sensitivities, Communication Studies, Celiac Disease Alternativecook.com Dedication This book is dedicated first to my husband, Mark my champion in life. Thank you for giving me so many enriching experiences. Second, I dedicate this book to the survey respondents and interview participants. Thank you for providing courageous examples of life with celiac disease and food sensitivities. Your interviews made me feel less alone, and gave me the confidence to forge ahead with this book. I think of you often and am so grateful that we can unite as a community. It is my sincere hope that this book can break down some of the social hurdles by bringing light to them. Creating awareness and having language to describe it are the first steps to making a positive change. Acknowledgements I’d like to take a moment to thank Heather, my editor for being my muse and for helping me to find and express my “voice” throughout. Thank you for your incredible patience as I learned the art of writing. I have loved our sessions and your insight! Thank you to Scott Adams at celiac.com for allowing me to post the survey, and to write about social scenarios these past few years. Thank you to my sister, Becky for your friendship and support. Thank you to my friends, Wendy, Marcia, Lori, Laura, Barbara, Jana, Kelley, Doreen, Sandy, the Literari Sisters, and my philanthropic Sisters who have given me support throughout. Thank you to my doctoral committee, Christina, Kate, Beth, and Nicole. I love you all, and thank you for your kind, loving understanding as I struggled with the disease to navigate life. Back to: Gluten-Centric Culture: Chapter 9 - Travel Tips Restaurant Primer
- 2 comments
-
- americans with disabilities act
- celiac disease
- (and 7 more)
-
Celiac.com 01/25/2020 - Depending on what source you read, there may be as many as 6.5 million celiac patients in the U.S. With these numbers, I have long believed that we really need to either find a cure or an effective way to manage this disease. I, like many others, have been wondering if a "magic pill" would ever be produced so I could escape from the dry, terrible tasting, overpriced gluten-free food. Thus, when I read an article about some research being done on celiac disease, I contacted the company conducting the clinical trials so I could be placed on their mailing list and hear about the results as soon as possible. At the time, I was not eligible to participate. To my surprise, a few months later, I was contacted by the agency conducting these trials. They asked if I would like to participate in the next testing phase of a medication called Larazotide which was being produced by Alba Pharmaceuticals. Prior to this opportunity, my only contribution to the celiac community was my list of foods that were actually palatable, and which I sent to newly diagnosed celiac sufferers on request. I also talked to my local specialty stores to ask them to order certain brands of foods and discontinue a certain brand of baked good that tastes like sand. With the invitation to be involved in this research, I now felt that I had an opportunity to really weigh in on a potential cure for this disease and really make a difference. At the appointed time, I went in for my physical and briefing. After learning about the drug, the study, and what would be expected, I signed on. I took my meds as instructed and kept my bowel movement data on what was affectionately named my "Brown Berry". This device was supplied by the agency as well as follow up visits and what I considered the most important benefit, both a pre and post-study duodenal biopsy. I entered the program with some apprehension, but to my surprise, it went quite smoothly. Appointments were made at my convenience and the contract allowed participants to leave the study at any time. The physical examination and subsequent follow ups were thorough and I was made to feel like a valuable part of the study. This article is not a promotional piece for Alba Pharmaceuticals. I had not even heard of them until I got involved in the study. It is however, a promotional piece is for all of you reading this is to become or stay active in the celiac community. I know from experience that involvement in such activities encourages you to take an active interest in your health. Whether it’s speaking to store managers about carrying quality products to make your life a little easier or getting involved in a study, it is time to be proactive. Don’t wait for someone else to step up. When this study is published sometime around the first of the year, I will be very proud of my small contribution. Let’s hope Larazotide is our "magic pill" and we can start enjoying real food again. Until then, please step up to the plate and become proactive in our health. We all benefit from each others’ contributions.
- 2 comments
-
- alessio fasano
- at 1001
- (and 6 more)
-

Are Celiac Disease Drug Treatments Just a Pipe Dream?
Jefferson Adams posted an article in Additional Concerns
Celiac.com 09/21/2022 - The dream of creating a safe, effective drug that can help people with celiac disease to tolerate small amounts, or perhaps even large amounts, of gluten. Until its recent failure, 9 Meters' larazotide was the only celiac drug in Phase 3 clinical trials. The recent discontinuation of larazotide, based on disappointing interim results, highlights the unmet need for effective alternatives to a gluten-free diet for treating celiac disease. Larazotide's failure also opens the doors for current and future Phase 1 and Phase 2 celiac therapies to be first-to-market. It also highlights the lack of a good lineup of potential new drugs. The reality is that, with the collapse of several once promising candidates, the bench for viable alternative celiac disease treatments is shallow, at best. Current Celiac Disease Pipeline Therapies Include: Latiglutenase (ImmunogenX) PRV-015 (Provention Bio, Inc. with Amgen) TAK-101 (Takeda Pharmaceuticals) ZED-1227 (ZEDIRA GmbH) KAN-101 (Anokion SA) In an effort to assess the current and future alternatives for treating celiac disease without a gluten-free diet, data marketing company Spherix recently interviewed one-hundred US gastroenterologists, and conducted eight qualitative interviews to compile a report on the issue. Spherix has issued a recent report on the form gastroenterologists engaged in a thorough review of these pipeline product descriptions (based on publicly available clinical information for each product). The report assesses celiac diagnostic and treatment trends emerging, as well as physician reactions to potential therapies in the pipeline. The 2022 report reveals a greater sense of urgency from gastroenterologists versus the 2021 report. Indeed, the number of respondents in the 2022 survey who say that their celiac patient load has increased in the past year, is up by 60% over 2021. Read more at PRNewswire.com- 32 comments
-
Celiac.com 12/20/2018 - Intestinal permeability is thought to play a key role in the translocation of bacteria that lead to nonalcoholic fatty liver disease (NAFLD), a disorder in which fat accumulates in the liver. Intestinal permeability is also thought to play a significant role in the development of Nonalcoholic steatohepatitis (NASH). In a new preclinical study, a team of researchers affiliated with Innovate Biopharmaceuticals recently assessed the effects of larazotide acetate on intestinal permeability. Their data from that study show that larazotide has a marked effect on intestinal permeability. The company expects to see more data detailing the use of larazotide in combination with approved drugs liraglutide (VICTOZA®) and obeticholic acid (OCALIVA®), in development for treatment of NASH, by early 2019. Based on larazotide's ability to re-normalize intestinal permeability, the parent company plans to launch clinical development program targeted at NASH in 2019. In the most recent study, researchers evaluated the effects of larazotide in a model of NASH that develops from consumption of a specified diet, the DIAMONDTM mouse model. The pre-clinical model confirms NAFLD/NASH in response to a high fat, high sugar Western diet, including insulin resistance, obesity, which mirrors human disease progression and histopathology. As tested, larazotide triggered a clear reduction in gut barrier permeability, a known pathological abnormality in chronic liver diseases, specifically NASH. Any drug that can prevent or reduce gut permeability could be helpful in treating NASH. The company plans to share the complete NASH pre-clinical results for publication in 2019. According to Dr. Arun Sanyal, Professor and Chair, Division of Gastroenterology, Hepatology and Nutrition at the Virginia Commonwealth University (VCU) School of Medicine, "Increased intestinal permeability has been linked to many aspects of metabolic syndrome including type 2 diabetes and nonalcoholic fatty liver disease. The demonstration of reduced gut permeability with larazotide in the setting of diet-induced obesity opens up the possibility of modulating the outcomes of metabolic syndrome, including NASH, via this mechanism and warrants further development for these indications." Obviously, any drug that can reduce gut permeability could also have implications for the treatment of celiac disease. Look for celiac.com to bring you more news on efforts to develop treatments for NASH, NAFLD, and related conditions, as information becomes available. Read more at: Nasdaq.com
- 2 comments
-
- celiac
- celiac diease
-
(and 5 more)
Tagged with:
-
Celiac.com 01/23/2020 - Researchers at the University of Maryland, under Alessio Fasano, have, once more, expanded the boundaries of human knowledge. The implications of their most recent discovery may soon unlock the mysteries of several autoimmune conditions including celiac disease, inflammatory bowel disease, type 1 diabetes, multiple sclerosis, and some types of cancers. Their discovery and subsequent report of zonulin, in 2000, was an enormous step forward. It provided insight into one, perhaps the only, common mechanism that causes leaky gut. Until then, many theories about leaky gut were proffered but none could be substantiated. We only knew that some autoimmune diseases, bowel diseases, and food allergies (or delayed sensitivities as some call them) seemed to trigger a leaky gut. Many of those with food allergies seemed to get some relief from eliminating foods to which their immune systems reacted, but we really did not understand the process by which these allergenic substances and various diseases induced a leaky gut. However, with the discovery and subsequent characterization of zonulin, it quickly became clear that a leaky gut was an important precursor to the development of at least some forms of autoimmunity. Although many medical practitioners continue to express skepticism about the importance of a leaky gut, emerging research findings should soon quell their concerns. Subsequent pharmacological research by Alba Therapeutics suggests that we may soon be able to abolish the permeable intestine that underlies so many autoimmune and other debilitating conditions. Currently in clinical trials, Alba Therapeutics is finding that Larazotide Acetate (formerly AT 1001) is abolishing the inflammatory sequelae when individuals with celiac disease consume gluten. Healthy digestion involves absorption of tiny, digested particles into the epithelial cells that line the intestine. These particles are then passed out the other side of the cell and into the bloodstream. These cells line the gut and maintain tight junctions to provide a protective barrier, except when zonulin attaches at cellular receptors. That is when the cells move further apart, allowing larger, undigested molecules to bypass the epithelial cells. Larazotide is designed to capture excess zonulin, which is over-produced by genetically susceptible individuals in response to ingested gluten. This drug is designed to capture the excess zonulin proteins and waste them in fecal matter, rather than allowing them to attach at receptors on epithelial cells. It is by this means that Larazodide is designed to prevent the development of a leaky gut, regardless of the cause of excessive zonulin production. Readers familiar with my work will not be surprised to learn that I’m not planning on eating gluten anytime soon. But I’d sure like to be able to take a pill containing an otherwise harmless substance, when dining out, whether at restaurants or at friends’ homes. I’d also like a tool that will help me to identify any other foods against which I may be mounting an inflammatory immune response. I imagine getting up in the morning and eating a couple of pancakes made from bean flours that I’m currently not able to tolerate. If I take some Larazotide first, and I get through the morning without my typical reactions–bloated stomach and heartburn–then I’ll know both what the culprit is and what I can do if I really want to have a couple of bean flour pancakes one morning. Similarly (and much more importantly) it will provide people with a tool for helping them to determine whether they are experiencing symptoms of food allergies or if their discomfort is caused by something else. For instance, if someone is unsure whether their foggy thinking really is the result of eating gluten, they can try Larazotide for a couple of meals. If their foggy brain clears up, but returns when they stop Larazotide and eat a meal containing gluten, then they will know that food (probably gluten) is likely the culprit. They may wish to pursue further self-testing or laboratory testing to identify specific problematic foods. This drug may also provide a tool for investigating children with attention deficit disorders (ADHD). If food sensitivities are the underlying culprit, these children should behave and pay attention fairly normally after a period of taking Larazotide before they consume any foods. We currently have no idea just how long such an intervention might take, but I’m hoping that researchers will soon answer such questions. I recently attended a conference on Crohn’s and colitis. When talking about treatments, the primary issues under discussion were the impact of various drugs on individuals present. The patients present shared a wealth of pharmaceutical knowledge. There was also considerable discussion of research aimed at a cure. In fact, the hosting organization seems quite fixated on finding a cure in the very near future. What a boon it would be, for everyone concerned, if Larazotide turns out to be that cure! But we knew all of this before. In fact, I’ve detailed most of this information in previous issues. What is new, and intensely exciting, is that the research group at U. Maryland has now determined that zonulin not only functions to increase intestinal permeability and inflammation, it is also a precursor to haptoglobin 2, a marker of inflammation that is exclusive to human beings. No other primates produce this protein, and only 80% of humans produce it. Considerable research has connected sub-groups of this marker to a variety of cardiovascular diseases, a range of autoimmune conditions, and many cancers. Thus, the production of zonulin, which will ultimately mature into haptoglobin 2, is a feature of many more ailments than was previously imagined. Since Larazotide is designed to capture and waste zonulin in fecal matter, we will soon be able to see what impact this drug can have on a variety of autoimmune diseases–and it promises to offer a tremendous benefit by halting the leakage of undigested proteins into the bloodstream that may be triggering autoimmune reactions by a process known as molecular mimicry. But that isn’t all Larazotide might offer. It could also offer insight into what has been characterized as the plague of the Twentieth Century, cancer. These inflammatory markers, haptaglobin 2, are elevated in association with many cancers. If the inflammation proves to be a significant factor in the survival of tumors, we will be able to block its production and deny this substance to the cancerous tissues. If, on the other hand, these inflammatory markers help the immune system to destroy tumors, we know how to trigger its production (in 80% of humans) and autoimmunity can be deterred by intravenous feeding during treatment. Either way, there is genuine cause for hope. My money is on the former possibility. I suspect removal of excess zonulin will reduce malignancies, but that is because diet can play an enormous role in cancer. There is already considerable anecdotal evidence suggesting a ketogenic diet is a viable therapy for insulin sensitive cancers. Time magazine ran a feature article titled “Can a High Fat Diet Beat Cancer?” in their September 17, 2007 issue. (The greatest difficulty these researchers are encountering with these trials is dietary compliance. Another serious problem is that their ethical approval required that all conventional treatments be exhausted before beginning the dietary trial. Thus, many of their research subjects are very sick before they begin the diet. For these reasons, one of the universities has stopped running these trials despite some promising preliminary results.) Whichever way it goes, Larazotide may well lead to some dramatic advances in cancer research in the very near future. Larazotide may also help some type 1 diabetics turn back the clock. Those who undergo islet cell transplants can usually only expect a year or two of reduced insulin requirements before they return to their former status. Larazotide may be able to halt the autoimmune destruction of the islet cells which produce insulin, allowing individuals who undergo transplants to experience relatively normal lives, without worrying about balancing the size of their insulin injections with their carbohydrate intake. They may well be able to forego injections entirely for the rest of their lives. Individuals with various autoimmune diseases may be able to halt the progression of their illness and return to more normal lives. Those with multiple sclerosis, Crohn’s disease, some forms of arthritis, lupus, and a host of other ailments may be stopped in their tracks. There may even be hope that people like me, with chronic lung disease, will be able to begin rebuilding healthy lung tissues. Reduced haptoglobin 2 may result in reductions in inflammatory reactions to airborne allergens. This, in turn, may permit us to breathe well enough that we can exercise and build healthy lung tissues without scar tissues. I’m not suggesting that we will be able to return to our 25 year-old activities, but I believe we may be able to live more normal, more productive lives for whatever time we have left. Finally, Larazotide may even bring about reductions in the excess mortality found in the celiac disease and gluten sensitive community. We have a lot to be grateful for. The research group directed by Alessio Fasano is making enormous contributions to broadening medical understanding of celiac disease, expanding medical knowledge of autoimmunity and cancer, and increasing celiac awareness (see: Scientific American, August 2008, “Surprises from Celiac Disease” by Alessio Fasano). As I said at the beginning, “They’ve done it again!”
- 1 comment
-
- alessio fasano
- at 1001
- (and 6 more)
-
Celiac.com 02/04/2013 - Ever wonder what happens to all those celiac disease patients who volunteer to do a gluten-challenge in the name of science? Well, the short answer is that they likely suffer, and may incur gut damage, at least in the short term. A team of researchers looking for ways to reduce or eliminate that problem recently conducted a study using larazotide acetate, a first-in-class oral peptide that prevents tight junction opening, and may reduce gluten uptake and associated problems. The research team included C. P. Kelly, P. H. R. Green, J. A. Murray, A. DiMarino, A. Colatrella, D. A. Leffler, T. Alexander, R. Arsenescu, F. Leon, J. G. Jiang, L. A. Arterburner, B. M. Paterson, R. N. and Fedorak. They are affiliated with the Celiac Center of Beth Israel Deaconess Medical Center at Harvard Medical School in Boston, the Celiac Disease Center at Columbia University in New York, NY, the Division of Gastroenterology and Hepatology at the Mayo Clinic in Rochester, MN, Thomas Jefferson University Hospital in Philadelphia, PA, the Pittsburgh Gastroenterology Associates in Pittsburgh, PA, with Gastrointestinal Specialists of Troy, MI, the Department of Internal Medicine at the University of Kentucky, in Lexington, KY, with Alba Therapeutics Corporation in Baltimore, MD, and with the Division of Gastroenterology at the University of Alberta in Edmonton, AB. The team wanted to find out how well larazotide acetate worked and how well it was tolerated by celiac disease patients undergoing a gluten challenge. To do this, the team conducted an exploratory, double-blind, randomized, placebo-controlled study that included 184 patients who maintained a gluten-free diet before and during the study. After a gluten-free diet run-in, the team randomly divided patients into groups and gave them either larazotide acetate in doses of 1, 4, or 8 mg three times daily, or a placebo. Both groups also received 2.7 grams of gluten daily for six weeks. The team then assessed ratios of lactulose-to-mannitol (LAMA), an experimental biomarker of intestinal permeability, and measured clinical symptoms by Gastrointestinal Symptom Rating Scale (GSRS) and anti-transglutaminase antibody levels. They found no significant differences in LAMA ratios between larazotide acetate and placebo groups. Larazotide acetate 1-mg limited gluten-induced symptoms measured by GSRS (P = 0.002 vs. placebo). They did find that the average ratio of anti-tissue transglutaminase IgA levels was 19.0 over baseline in the placebo group compared with 5.78 (P = 0.010) in the 1mg larazotide acetate group, 3.88 (P = 0.005) in the 4mg larazotide acetate group, and 7.72 (P = 0.025) in the 8mg larazotide acetate group. Both the larazotide acetate and placebo groups showed similar rates of "adverse events." Overall, the team found that larazotide acetate reduced gluten-induced immune reactivity and symptoms in celiac disease patients undergoing gluten challenge and was generally well tolerated. However, the team found no significant difference in LAMA ratios between the larazotide acetate and placebo groups. Even though they did not find anything revolutionary, the results and design of their study will likely be helpful in shaping future gluten-challenge studies in patients with celiac disease. Source: Aliment Pharmacol Ther. 2013;37(2):252-262.
- 2 comments
-
Celiac.com 11/21/2022 - Following a gluten-free diet for life can be difficult, Most celiacs on a gluten-free diet get exposed to gluten on a regular basis, especially if they eat in restaurants. Currently, a gluten-free diet is the only effective treatment for celiac disease. Because of this, there is substantial interest in drug therapies that can help to protect celiacs on a gluten-free diet, and, ideally, free them from a strict gluten-free diet. There are a number of drugs still in the pipeline that promise the former, at least. So what's the status of the multiple new therapies that are under investigation? To answer this question, a team of researchers recently set out to review existing and upcoming clinical trial programs for pharmacologic agents for celiac disease. The team conducted a narrative review using searches of MEDLINE, Embase, the Cochrane CENTRAL Library and clinicaltrials.gov. In their review, the team summarizes the pathophysiology of celiac disease, and the specific steps that might help to speed pharmacologic treatment. They also assess the evidence in support of current and future drug targets, including trials of peptidases, gluten sequestrants, tight junction regulators, anti-transglutaminase 2 therapies, immune tolerizing agents, advanced biologics and small molecules, and microbiome-targeted strategies. The team also spotlights the special challenges of conducting celiac disease trials, including identifying appropriate study populations, assessing results in the context of a gluten challenge, and interpreting celiac disease-specific clinical and histologic outcomes. Understanding these factors is crucial for accurately appraising the evidence. Finally, they outline what the future of celiac disease therapy may hold with the introduction of viable drug treatments. There is a definite need for drug options for treating celiac disease, either for accidental or intentional gluten exposures, as part a gluten-free diet, or for refractory disease. The big takeaway, is that, according to the team's reading of the data, multiple promising celiac disease drug therapies are in development, and these trials are likely to lead to approvals for the first generation of pharmacologic agents for celiac disease within the next 5 years. Color us skeptical, but that seems a pretty bullish view, especially given the crowded graveyard of once seemingly promising celiac drug therapies, especially the very recent demise of the highly touted Larazotide. Basically, we'll believe in successful drug treatments for celiac disease when we see a successful product make it to celiacs. Meanwhile, stay tuned for more on this and related stories. Read more in Aliment Pharmacol Ther. 2022;55(10):1277-1296 The research team included Michael Klonarakis, Christopher N. Andrews, Maitreyi Raman, Remo Panaccione and Christopher Ma. They are variously affiliated with theDepartment of Medicine, University of Calgary, Calgary, Alberta, Canada; the Division of Gastroenterology & Hepatology, University of Calgary, Calgary, Alberta, Canada; the Alberta's Collaboration of Excellence for Nutrition in Digestive Diseases, Calgary, Alberta, Canada; and the Department of Community Health Sciences, University of Calgary, Calgary, Alberta, Canada.
- 11 comments
-
- celiac disease
- diet
- (and 6 more)
-

Are Celiac Disease Drug Treatments Just a Pipe Dream?
Guest commented on Jefferson Adams's article in Additional Concerns
I recently wrote this article for Dutch celiac disease patients (translated with Google): Research into medicines for celiac disease A drug to treat celiac disease? Some are looking forward to it. For others it is not necessary, they can manage just fine with a gluten-free diet. For the group that has difficulty with the gluten-free diet, because it has such a major impact on daily life, because complaints remain, or the intestines do not recover properly, a medicine is being sought in various countries. This can be a new drug, or a drug that is already being used for another disease. These are the main drugs currently being tested: 1. enzymes that should make gluten less harmful (AN-PEP, Latiglutenase, TAK-062) 2. Injections with substances that reprogram the immune system to accept gluten (TAK-101) 3. a German drug that disables the enzyme tissue transglutaminase (TTG), so that the small intestine is no longer damaged after eating gluten (ZED1227) 4. a drug to reduce inflammation (PRV-015); the Amsterdam UMC is one of the many hospitals in the world where this drug is tested in celiac patients 5. the drug teriflunomide, originally intended for the treatment of MS, is being tested in Norway by a small group of celiac patients; they are allowed to eat gluten for three days and receive either the drug or a placebo (fake drug). It is being investigated whether celiac patients who receive the MS drug become less ill. These drugs are dots on the horizon for patients with celiac disease. They beckon, but at the same time they are still far away. The development of a drug, for any disease, takes years. And many initiatives that at first seemed promising, fail along the way, because they are not as good as hoped (Nexvax2 and Larazotide are examples of this). The gluten-free diet sets the bar high: a new treatment must be at least as good, and preferably even better. Now we just have to wait and see what the future brings, whether there is a drug in between that makes it to the finish line. Source: Dieckman T, Koning F, Bouma G. Celiac disease: New therapies on the horizon. Curr Opin Pharmacol. 2022 Jul 31; 66:102268. doi: 10.116/j.coph.2022.102268.- 32 comments
-
Celiac.com 06/16/2021 - Weeks after SARS-CoV-2 infection or exposure, some children develop a severe, life-threatening illness called Multisystem Inflammatory Syndrome in Children (MIS-C). A new study offers hope for diagnosis, treatment and prevention of MIS-C. Gastrointestinal symptoms are common in MIS-C patients and severe hyperinflammatory response ensues with potential for cardiac complications. The cause of MIS-C has not previously been identified. A team of researchers recently set out to learn more about diagnosing, treating, and preventing MIS-C. The research team analyzed specimens from 19 children with MIS-C, 26 with acute COVID-19, and 55 control subjects and assessed stool samples for SARS-CoV-2 by RT-PCR, and plasma samples for markers of breakdown of mucosal barrier integrity, including zonulin. They used ultra-sensitive antigen detection to probe for SARS-CoV-2 antigenemia in plasma, and then characterized the resulting immune responses. As proof of concept, we treated a MIS-C patient with larazotide, a zonulin antagonist, and monitored impact on antigenemia and clinical response. The team demonstrated that, in MIS-C patients, prolonged presence of SARS-CoV-2 in the GI tract leads to the release of zonulin, an intestinal permeability biomarker, which causes SARS-CoV-2 antigens to flow into the bloodstream, and triggers hyperinflammation. The one MIS-C patient treated with larazotide, a drug which is currently in clinical trials as a possible treatment for celiac disease, showed a coinciding decrease in plasma SARS-CoV-2 Spike antigen levels, inflammatory markers, along with clinical improvement above that resulted from presently available treatments. The team's data detailing the pathogenesis of MIS-C offers insight into targets for diagnosing, treating, and preventing MIS-C, which are crucial to addressing this increasingly common severe COVID-19-related disease in children. Read more at The Journal of Clinical Investigation. The research team included Lael M. Yonker, Tal Gilboa, Alana F. Ogata, Yasmeen Senussi, Roey Lazarovits, Brittany P. Boribong, Yannic C. Bartsch, Maggie Loiselle, Magali Noval Rivas,4 Rebecca A. Porritt,4 Rosiane Lima,1 Jameson P. Davis, Eva J. Farkas, Madeleine D. Burns, Nicola Young, Vinay S. Mahajan, Soroush Hajizadeh, Xcanda I. Herrera Lopez,5 Johannes Kreuzer, Robert Morris, Enid E. Martinez, Isaac Han, Kettner Griswold Jr., Nicholas C. Barry, David B. Thompson, George Church, Andrea G. Edlow, Wilhelm Haas, Shiv Pillai, Moshe Arditi, Galit Alter, David R. Walt, and Alessio Fasano. They are variously affiliated with the Department of Pediatrics, Massachusetts General Hospital, Boston, United States of America; the Department of Pathology, Brigham and Women’s Hospital, Boston, United States of America; the Department of Medicine, Ragon Institute of MGH, MIT and Harvard, Cambridge, United States of America; the Department of Pediatrics, Cedars-Sinai Medical Center, Los Angeles, United States of America; the Department of Medicine, Massachusetts General Hospital, Boston, United States of America; the Department of Immunology, Wyss Institute for Biologically Inspired Engineering, Boston, United States of America; the Department of Genetics, Harvard Medical School, Boston, United States of America; the Department of Obstetrics, Gynecology, and Reproductive Biology, Massachusetts General Hospital, Boston, United States of America; the Massachusetts General Hospital, Boston, United States of America; the Department of Immunology, Massachusetts General Hospital, Boston, United States of America; and the Department of Pathology, Harvard Medical School, Boston, United States of America.
-

How Close Are New Celiac Disease Treatments?
Jefferson Adams posted an article in Diagnosis, Testing & Treatment
Celiac.com 04/10/2015 - Of course, a strict gluten free diet is still the only safe and effective treatment for celiac disease. However, new drugs in development, some of which are currently being tested on humans, might allow people with celiac disease to safely eat gluten again, at least in small amounts. To be fair, even if all goes smoothly, it will be a few years at least before we see such treatments on the market. Moreover, even though many early results have been encouraging, none have yet entered safety trials, the final step before Food and Drug Administration approval and commercial availability. Drugs currently under trial include an enzyme that splits the protein in wheat that triggers adverse reactions, into smaller harmless products, and another which promises to make the gut less leaky, and thus block potentially toxic substances from triggering inflammation. There are several other drugs in earlier stages of development aimed at suppressing the immune response to gluten and preventing intestinal inflammation: ALV003, which will protect people with celiac disease against gut damage from small amounts of gluten. BL-7010 is a novel co-polymer for the treatment of celiac disease, which significantly reduces the immune response triggered by gluten. ImmusanT’s therapeutic vaccine Nexvax2 combines three proprietary peptides that elicit an immune response in celiac disease patients who carry the immune recognition gene HLA-DQ2. Larazotide acetate (AT-1001) is Alba Therapeutics Corporation’s investigational product, a first-in-class tight junction regulator, intended for the treatment of patients with celiac disease. AVX176, from Avaxia Biologics, is an investigational oral antibody drug that is the subject of U.S. composition of matter patent 8,071,101, “Antibody Therapy for Treatment of Diseases Associated with Gluten Intolerance.” The patent, which expires on May 27 2029, provides broad coverage for treating celiac disease using orally administered antibodies produced by Avaxia’s proprietary platform technology [32]. ActoGenX is carrying out discovery research in celiac disease with its range of ActoBiotics™, which use Lactococcus lactis as an expression system to locally secrete bio-therapeutics such as cytokines, antibodies, hormones, etc. Chemocentryx’s CCR9, is also known as Traficet-EN, or CCX282B), and was originally intended for patients with moderate-to-severe Crohn’s disease. It has completed one Phase 2 trial in 67 patients with celiac disease. Meanwhile, in Europe, Dr. Falk Pharma and Zedira recently announced the start of phase I clinical trials for the drug candidate ZED1227, a direct acting inhibitor of tissue transglutaminase. The small molecule targets the dysregulated transglutaminase within the small intestine in order to dampen the immune response to gluten which drives the disease process. Some of these drugs may be taken right before eating gluten, while others might be more effective when taken on a regular schedule. If approved for use as intended, these drugs will likely allow people with celiac disease to eat gluten in small amounts. To my knowledge, there is no drug in current trial phases that is designed to permit unrestricted gluten consumption. So, the good news is that the next few years may see commercially available treatments that might actual help people manage celiac disease. The downside for people with celiac disease, at least for now, is that there is no treatment on the horizon that will allow safe, unlimited gluten-consumption. Moreover, there is no hint that a cure is coming anytime soon. Still, it’s good to know that researchers are working on providing helpful tools for treating celiac disease. Are you looking forward to seeing new treatment options for celiac disease? What kind of benefits should such treatments offer? Source: Gastroenterology Report- 18 comments
-
- celiac
- celiac disease
-
(and 3 more)
Tagged with:
-
Celiac.com 04/04/2016 - Any one eager to try the first approved treatment for celiac disease might not have to wait much longer. Alba Therapeutics has announced that their celiac treatment, larazotide acetate, will enter the first Phase 3 clinical trials ever conducted in a celiac disease drug later this year. Lorazotide acetate works by improving regulation of tight junctions in the bowel. In healthy people, these junctions remain closed except to shed dead cells, but in patients with celiac disease, gluten keeps tight junctions open, triggering an inflammatory reaction that eventually destroys the intestinal villi, tiny, finger-like projections in the small intestine that are essential for nutrient absorption. Early research suggests larazotide acetate helps to keep the tight junctions closed when it's taken before a meal, thus stopping, or reducing the reaction and the resulting inflammation. Larazotide acetate recently completed during phase 2b clinical trials for efficacy, safety and tolerability in 342 patients with celiac disease. Those trials showed larazotide acetate to be safe and effective in a "real world setting" for celiac patients, according to Alba's website. The treatment is now headed to Phase 3 trials in "late 2016", and has received "fast track" designation from the Food and Drug Administration. Alba has announced that Innovate Biopharmaceuticals Inc. has licensed all of Alba Therapeutics' assets related to larazotide acetate, and that larazotide acetate has been renamed INN-202. If approved on schedule, INN-202 will become the first prescription medicine for treating celiac disease. Source: Allergic Living
- 11 comments
-
- celiac
- celiac disease
-
(and 7 more)
Tagged with:
-
Celiac.com 01/14/2019 - There are a number of new drugs in development that are designed to treat celiac disease. In addition to a possible vaccine, those drugs include enzymes and other drugs that are designed to reduce or eliminate the body’s adverse reaction to gluten through various mechanisms. Here's a 2019 status update for every drug for treating celiac disease currently in development: ALV003—Created by Alvine Pharmaceuticals, is a combination of two enzymes that break down gluten before it can provoke an immune reaction. The drug is a powder to be dissolved in water and taken before meals. ALV003 passed a phase 2 clinical trial, and results were published in the June 2014 issue of Gastroenterology. Post-trial biopsies showed that ALV003 prevented intestinal damage in 34 volunteers with celiac disease, each of whom ate 2 grams of gluten per day for six weeks, in addition to taking ALV-003. Phase 2b, a 12-week trial, is now underway. AN-PEP (aspergillus niger prolyl endopeptidase)—Created by DSM Food Specialties, AN-PEP is another enzyme that degrades gluten. AN-PEP is believed to work best when taken while gluten is still in the stomach. A 2013 study showed AN-PEP to be safe, but failed to show that the enzyme had any effect, so further study is under way. That study appeared in the World Journal of Gastroenterology. In a 2018 study, AN-PEP extensively degraded gluten concentrations of up to 80,000 mg/kg in rye flour, rye sourdough, and sourdough starter under specific temperatures and pH values, while leaving the microorganisms in the sourdough starter fully intact. ActoBiotics—Created by ActoGenX uses Lactococcus lactis as an expression system to locally secrete bio-therapeutics such as cytokines, antibodies, hormones, etc. Early pre-clinical work with a genetically altered L. lactis secreting a peptide derived from gliadin demonstrated an in vivo suppression of gluten sensitization. Specifically, Huigbregtse et al. engineered L. lactis to secrete a deamidated DQ8 gliadin epitope (LL-eDQ8d) and studied the induction of Ag-specific tolerance in NOD ABo DQ8 transgenic mice [34]. Although apparently not part of the ActoGenX development program, recent work by Galipeau et al. also deserves mention in this context. The group treated gluten-sensitive mice with elafin, a serine protease inhibitor, delivered by the L. lactis vector, and found normalization of inflammation, improved permeability, and maintained ZO-1 expression. There is speculation that this is due to reduced deamidation of gliadin peptide. AVX176—Created by Avaxia Biologics, is an investigational oral antibody drug patented to provide "Antibody Therapy for Treatment of Diseases Associated with Gluten Intolerance." The patent, which expires on May 27 2029. AVX176 provides broad coverage for treating celiac disease using orally administered antibodies produced by Avaxia's proprietary platform technology. BL-7010—by BioLineRx, is a novel co-polymer for the treatment of celiac disease, which significantly reduces the immune response triggered by gluten. This drug has been shown in mice to reduce the immune system response that leads to intestinal damage and villous atrophy in celiac disease. BL-7010 actually binds to the gluten protein, reducing the protein's toxicity.The drug, with the gluten molecule attached, then passes harmlessly through the digestive system to be expelled as stool. BL-7010 has undergone safety testing in humans and was found to be well tolerated. According to BioLineRx, testing will begin in mid-2015 to see if the drug works as expected to diminish gluten's effects on the body. However, BL-7010 is designed to protect only against gluten cross-contamination; it won't allow people with celiac disease to eat large amounts of gluten. CCR9—by Chemocentryx, is a drug called vercirnon, which is also known as Traficet-EN, or CCX282B), and was originally intended for patients with moderate-to-severe Crohn's disease. CCR9 has completed one Phase 2 trial in 67 patients with celiac disease. However, despite the completion of the trial several years ago, no results relating to celiac disease have been made public or published. Egg Yolk Enzyme—Little is known about efforts to develop a celiac treatment that uses egg yolk to coat gluten and allow it to pass through the body undetected, thus preventing an adverse gluten reaction in sensitive individuals. Like most other drugs being developed, this treatment would work to prevent reactions to small amounts of gluten, rather than as a cure for celiac disease. Recent news shows that the egg yolk enzyme is safe for humans. GliadinX (Aspergillus niger)—GliadinX is a dietary supplement with the highest concentration of AN-PEP, Prolyl Endopeptidase (Aspergillus Niger), the most effective enzyme proven to break down gluten in the stomach. This high potency enzyme formulation is specifically designed to break down gliadin. GliadinX does not prevent or cure celiac disease. However, clinical research has shown that it effectively breaks down gliadin into small, harmless fragments before it can reach the small intestine. INN-202 (Larazotide Acetate)—Created by Alba Therapeutics and later acquired by Innovate Pharmaceutical, and renamed INN-202, larazotide acetate works by blocking a protein that carries pieces of gluten across the gut. Results of a phase 2 trial of larazotide acetate appear in the February 2015 edition of Gastroenterology. While INN-202 may greatly reduce the symptoms of gluten exposure in celiacs, it is unlikely that a permit consumption of unlimited amounts of gluten. The U.S. Food and Drug Administration (FDA) has fast-tracked the drug. Phase III clinical trials are currently underway. Results of the trial should be available soon. Nexvax2—Created by ImmusanT, Nexvax2 is touted as a vaccine, but works much like an allergy shot. Nexvax2 combines three proprietary peptides that elicit an immune response in celiac disease patients who carry the immune recognition gene HLA-DQ2. Similar to allergy shots, the vaccine is designed to reprogram gluten-specific T cells triggered by the patient's immune response to the protein. Nexvax2 exposes the immune system to gluten in a controlled way so that immune cells that are usually activated get turned off or eliminated. So far, Nexvax2 has completed a phase 1 trial showing it to be safe, and the company has begun Phase II trials on humans in Australia and New Zealand. Saliva Rothia—Researchers at the Henry M. Golden School of Dental Medicine were looking at how proteins in general break down in saliva when they discovered an enzyme in a bacterium called Rothia that pulverized gluten as if it were Pac Man. That happy accident has led to a new stream of study that has moved beyond petri dishes to study the effect of the so-called ‘subtilisin,’ or protein-ingesting enzyme on the tiny digestive systems of mice. In so doing, they have found another bacterium, B. subtilis, which produces an enzyme similar to the Rothia one and is already safely consumed in Japan in a fermented soybean dish called ‘natto.’ A 2018 Boston University report concludes that “oral Rothia bacteria to gliadin digestion and pharmaceutical modification can protect Sub-A from auto-digestion as well as from acidic insults, thus rendering the usefulness of coated subtilisins as a digestive aid for gluten degradation.” ZED1227—Created by Dr. Falk Pharma and Zedira recently announced the start of phase II clinical trials for the drug candidate ZED1227, a direct acting inhibitor of tissue transglutaminase. ZED1227 molecules work by targeting the dysregulated transglutaminase within the small intestine in order to suppress the immune response to gluten which drives the disease process. Sources: An Update on Every Celiac Disease Drug Currently in Development Inside The Race for a Celiac Disease Treatment Promising Celiac Disease Drugs in the Pipeline Development of drugs for celiac disease: review of endpoints for Phase 2 and 3 trials
- 2 comments
-
- celiac
- celiac disease
- (and 6 more)
-

Are Enzymes Effective Against Gluten Contamination?
Dr. Albert Zickmann posted an article in Spring 2020 Issue
Celiac.com 03/06/2020 - Celiac disease has an incidence of about 1% in the general population. It is an automimmune disease triggered by a proline-rich protein, gliadin, when it enters the small intestine and leaks into the wall of the small intestine (therefore the name leaky gut). Humans cannot break down proline-rich proteins. In healthy persons, gliadin passes through the gastrointestinal tract and is excreted in stool and urine without consequences. Celiac patients, build antibodies in the small intestine and these antibodies travel through the blood stream in all areas of the body. In some patients, there are no apparent symptoms or they can be very mild, while in others the symptoms are quite severe and are even associated with an increased risk of a certain type of intestinal cancer. Researchers have identified that the body breaks down some of the components of gliadin, but the human body cannot break down and digest the components that contain the amino acid proline. There are two such segments of the gliadin molecule that are causing an inflammatory reaction and they are called 33-mer and 26-mer peptides, because they contain a 33 and respectively a 26 amino acid sequence. In an effort to prevent the gliadin molecule from leaking into the wall of the small intestine, a variety of methods have been tried. These include, closing the junctions through which gliadin leaks, encapsulating the gliadin molecule, and enzymatic degradation of the inflammatory segments of the gliadin molecule. The smallest protein chain that can cause an inflammatory reaction is 9 amino acids long, and the goal would be to break down the gliadin molecule in segments of 8 or less amino acids. This has to happen before the gliadin molecule enters the small intestine and leak into the wall of the intestine. The most commonly sold over-the counter enzymes are in the DPP-IV group, and while they are in fact very effective in breaking down gliadin's smaller segments, they cannot break down the proline rich areas in segments of less than 9 amino acids, and are therefore not effective in preventing an inflammatory reaction. The three enzymes that have shown promising results are ALV003, an enzyme combination of 2 enzymes that is currently undergoing FDA testing, AN-PEP, produced by DSM, and enzyme that was originally used to make cold brewed beer clear, and a product called KumaMax, purchased by Takeda Pharmaceuticals. At this time only AN-PEP is available in various concentrations on the market. It has been particularly effective at breaking down gluten at a low pH commonly found in the stomach, and a study has shown that AN-PEP is even more effective if combined with a food grade acid. The tests were done in healthy volunteers and under laboratory conditions and several groups of researchers came to the same conclusions that AN-PEP is very effective in cleaving the gliadin molecule. The tests are considered pertinent even if healthy volunteers were selected because enzymes work in the stomach and not systemically and in that respect, there is no difference between a celiac patient and a healthy individual. Until a few years ago, gluten-sensitivity was considered to have the same cause as celiac disease, namely the gliadin molecule and in order to avoid regulator issues, these enzymes were recommended only for gluten sensitivity but not for celiac disease. Recent work suggests that these enzymes are in fact not as effective for gluten sensitivity because the culprit of most gluten sensitivities might not be the gliadin molecule. Enzymes Do Not Change the Nature of Celiac Disease and Do Not Treat or Cure It Existing data is very encouraging and clearly proves that AN-PEP enzymes greatly reduce the concentration of gliadin and can possibly even make it undetectable. It is important to note, that these enzymes do not change the nature of celiac disease and therefore do not treat or cure it. They can only break down the molecule that is triggering a reaction and therefore help maintain a gluten-free diet when contaminants are present. Essentially, there are two ways to maintain a gluten-free diet. One way is to avoid any contaminants in the food but most authorities agree that this is almost unattainable. The second way, is to break down the contaminants before they can cause damage. The underlying immune-deficiency is not changed and adherence to a gluten-free diet can not be neglected. Clinicians are reluctant to recommend enzymes for gluten contamination and certainly not for intentional consumption without regulatory approval. The big challenge is that short term gluten challenge studies have been inconclusive because they did not prove an advantage over a placebo. In order to obtain conclusive results, patients who have been on a gluten-free diet for months or even for years before they develop symptoms or antibodies, and therefore a study to prove conclusively an advantage over a placebo, is very difficult to conduct and might take years. Given this challenge, it is unlikely that an enzyme will ever go through the FDA process. As long as enzymes are not recommended to treat or cure a disease, they do not have to be FDA approved but are regulated by the FDA and have to be registered as dietary ingredients. Enzymes Could Lead to Being Less Careful and Cause a Higher Risk of Gluten Exposure There is the concern that enzymes could lead to being less careful and therefore causing a higher risk of gluten exposure, and this is a valid argument, but the ethical question then arises whether this is enough reason to withhold the additional benefit of safety to those who are careful. A recent study suggests that there is a method to measure the impact of gluten with a blood test of interleukin-2 within a few hours of gluten ingestion, and the results could make a gluten-challenge study shorter and safer and could help investigate enzymes or other methods that support a gluten-free diet. Another very promising application for enzymes is to treat gluten-containing food products and break down the immunogenic components of gliadin. These foods could not be labeled as gluten-free but only as gluten-removed. It is currently accepted that alcoholic drinks such as vodka or whiskey that are made from gluten containing grains are considered safe because of the distillation process that removes all gluten-proteins from the final product. Current laboratory tests are very accurate in determining if a product does or does not contain gluten. Currently an enzymatically treated product is not considered at the same level of safety as when gluten (gliadin molecule) is completely removed from a food product. However, at least theoretically, there should be no difference between a product that is made from non-gluten containing ingredients and a product that has been treated in a way that the finished product has no detectable gluten molecules. In conclusion, evidence is very strong that enzymes could be recommended for the breakdown of contaminants in support of a gluten-free diet, but not to replace a gluten-free diet. This does greatly enhance the quality of life for celiac patients when eating outside of a completely controlled environment, which is not attainable for most people. Join the forum discussion on on enzymes discussed in this article. Studies on AN-PEP: Extra-Intestinal Manifestation of Celiac Disease in Children. Nutrients 2018, 10(6), 755; doi:10.3390/nu10060755 Efficient degradation of gluten by a prolyl endoprotease in a gastrointestinal model Enzymatic gluten detoxification: the proof of the pudding is in the eating! Highly efficient gluten degradation with a newly identified prolyl endoprotease: implications for celiac disease Degradation of gluten in wheat bran and bread drink by means of a proline-specific peptidase References: Hausch, F., Shan, L., Santiago, N. A., Gray, G. M. & Khosla, C. Intestinal digestive resistance of immunodominant gliadin peptides. Am. J. Physiol. Gastrointest. Liver Physiol. 283, G996–G1003 (2002) Shan, L. et al. Structural basis for gluten intolerance in celiac sprue. Science 297, 2275–2279 (2002) Greco, L. et al. Safety for patients with celiac disease of baked goods made of wheat flour hydrolyzed during food processing. Clin. Gastroenterol. Hepatol. 9, 24–29 (2011) Stoven, S., Murray, J. A. & Marietta, E. Celiac disease: advances in treatment via gluten modification. Clin. Gastroenterol. Hepatol. 10, 859–862 (2012) Gass, J. & Khosla, C. Prolyl endopeptidases. Cell. Mol. Life Sci. 64, 345–355 (2007) Mitea, C. et al. Efficient degradation of gluten by a prolyl endoprotease in a gastrointestinal model: implications for coeliac disease. Gut 57, 25–32 (2008) Shan, L., Marti, T., Sollid, L. M., Gray, G. M. & Khosla, C. Comparative biochemical analysis of three bacterial prolyl endopeptidases: implications for coeliac sprue. Biochem. J. 383, 311–318 (2004) Edens, L. et al. Extracellular prolyl endoprotease from Aspergillus niger and its use in the debittering of protein hydrolysates. J. Agric. Food Chem. 53, 7950–7957 (2005) Marti, T. et al. Prolyl endopeptidase-mediated destruction of T cell epitopes in whole gluten: chemical and immunological characterization. J. Pharmacol. Exp. Ther. 312, 19–26 (2005) Stepniak, D. et al. Highly efficient gluten degradation with a newly identified prolyl endoprotease: implications for celiac disease. Am. J. Physiol. Gastrointest. Liver Physiol. 291, G621–G629 (2006) Pyle, G. G. et al. Effect of pretreatment of food gluten with prolyl endopeptidase on gluten induced malabsorption in celiac sprue. Clin. Gastroenterol. Hepatol. 3, 687–694 (2005) Gass, J., Vora, H., Bethune, M. T., Gray, G. M. & Khosla, C. Effect of barley endoprotease EPB2 on gluten digestion in the intact rat. J. Pharmacol. Exp. Ther. 318, 1178–1186 (2006) Bethune, M. T. et al. A non-human primate model for gluten sensitivity. PLoS ONE 3, e1614 (2008). 29. Siegel, M. et al. Rational design of combination enzyme therapy for celiac sprue. Chem. Biol. 13, 649–658 (2006) Gass, J., Bethune, M. T., Siegel, M., Spencer, A. & Khosla, C. Combination enzyme therapy for gastric digestion of dietary gluten in patients with celiac sprue. Gastroenterology 133, 472–480 (2007) Siegel, M. et al. Safety, tolerability, and activity of ALV003: results from two phase 1 single, escalating-dose clinical trials. Dig. Dis. Sci. 57, 440–450 (2012) Tye-Din, J. A. et al. The effects of ALV003 predigestion of gluten on immune response and symptoms in celiac disease in vivo. Clin. Immunol. 134, 289–295 (2010) Lähdeaho, M. L. et al. ALV003, a novel glutanase, attenuates gluten-induced small intestinal mucosal injury in coeliac disease patients: a randomized controlled phase 2a clinical trial. Gut Suppl. 60, A12 (2011) Janssen, G. et al. Ineffective degradation of immunogenic gluten epitopes by currently available digestive enzyme supplements. PLos One 10, e0128065 (2015). Stenman, S. et al. Enzymatic detoxification of gluten by germinating wheat proteases: implications for new treatment of celiac disease. Ann. Med. 41, 390–400 (2009) Stenman, S. et al. Degradation of coeliac disease-inducing rye secalin by germinating cereal enzymes: diminishing toxic effects in intestinal epithelial cells. Clin. Exp. Immunol. 161, 242–249 (2010) Laparra, J. M. & Sanz, Y. Bifidobacteria inhibit the inflammatory response induced by gliadins in intestinal epithelial cells via modifications of toxic peptide generation during digestion. J. Cell. Biochem. 109, 801–807 (2010) De Angelis, M. et al. VSL#3 probiotic preparation has the capacity to hydrolyze gliadin polypeptides responsible for celiac sprue. Biochim. Biophys. Acta 1762, 80–93 (2006) Julia König et al. Is an enzyme supplement for celiac disease finally on the cards? Pages 531-533 | Received 01 Feb 2018, Accepted 02 May 2018, Accepted author version posted online: 06 May 2018, Published online: 11 May 2018 Pinier, M. et al. Polymeric binders suppress gliadin-induced toxicity in the intestinal epithelium. Gastroenterology 136, 288–298 (2009) Pinier, M. et al. The copolymer P(HEMAcoSS) binds gluten and reduces immune response in gluten-sensitized mice and human tissues. Gastroenterology 142, 316–325 (2012) Smecuol, E. et al. Gastrointestinal permeability in celiac disease. Gastroenterology 112, 1129–1136 (1997) Tripathi, A. et al. Identification of human zonulin, a physiological modulator of tight junctions, as prehaptoglobin2. Proc. Natl Acad. Sci. 106, 16799–16804 (2009) Lammers, K. M. et al. Gliadin induces an increase in intestinal permeability and zonulin release by binding to the chemokine receptor CXCR3. Gastroenterology 135, 194–204 e193 (2008) Di Pierro, M. et al. Zonula occludens toxin structure-function analysis. Identification of the fragment biologically active on tight junctions and of the zonulin receptor binding domain. J. Biol. Chem. 276, 19160–19165 (2001) Leffler, D. A. et al. A randomized, double-blind study of larazotide acetate to prevent the activation of celiac disease during gluten challenge. Am. J. Gastroenterol. 107, 1554–1562 (2012) Kelly, C. P. et al. Larazotide acetate in patients with coeliac disease undergoing a gluten challenge: a randomised placebo-controlled study. Aliment. Pharmacol. Ther. 37, 252–262 (2013) Katharina Anne et al. Novel approaches for enzymatic gluten degradation to create high-quality gluten-free products https://doi.org/10.1016/j.foodres.2016.11.021 -

Does New Drug Promise Cure for Celiac Disease?
Dr. Vikki Petersen D.C, C.C.N posted an article in Winter 2013 Issue
Celiac.com 06/23/2017 - Dr. Alessio Fasano from the University of Maryland's Celiac Research Center published a paper in Clinical and Developmental Immunology last month. It focused on a new drug developed by Dr. Fasano that has shown promising results in both animal and human trials. But is this the 'magic pill' that will cure celiac disease and gluten sensitivity? Let's take a look. The new drug, formerly called AT1001 but now renamed Larazotide Acetate, is a zonulin inhibitor. For those who have never heard the word 'zonulin', you might think it's a term from a science fiction movie. But zonulin is the protein that causes the 'gates' or openings between the cells making up the lining of the small intestine to open and close. These openings are called tight junctions and when zonulin gets excessive, a leaky gut ensues. Dr. Fasano has made great inroads to prove that a leaky gut is a problem that must be handled with gluten intolerance. The leaky gut perpetuates gluten's negative impact on other parts of the body. It can also initiate autoimmune disease. One key point to keep in mind is that 'leaky gut' occurs because molecules can pass between cells when they shouldn't. In addition, molecules can pass through cells which they also shouldn't. Unfortunately this new drug only impacts the former, not the latter. So, the drug Larazotide Acetate is a zonulin inhibitor. Now that we've reviewed what zonulin does as regards opening the gates, the purpose of inhibiting its action should make sense. How well does it work? In the recent human trials that were double-blind, randomized placebo-controlled (the best type of study, but I would expect no less from the stellar Dr. Fasano), a gluten exposure created a 70% increase in intestinal permeability (leaky gut) in 57% of the placebo group but only 28.6% of the patients receiving the drug (4 out of 14 patients) experienced such increased permeability. Further, gastrointestinal symptoms were significantly more frequent among patients of the placebo group as compared to the group that received the Larazotide. A pro-inflammatory substance known as interferon gamma was also evaluated. This is manufactured by the body when a specific foreign/toxic agent is recognized by the body's immune system. As expected, levels of interferon gamma increased in 4 out of 7 of the placebo patients (57%) but only 4 out of 14 larazotide patients (28.6%) saw any increase. The good news is that this drug seems well tolerated and it does reduce the leaky gut response that gluten ingestion normally creates. Further, it also reduces the percentage, by about half, of the production of interferon gamma. These are all excellent results. But, and it's unfortunately a very big 'but', we have a very long way to go before such a drug would be useful for your typical celiac or gluten sensitive patient. Will Dr. Fasano and his team be able to tweak this drug such that it functions at a higher level of efficacy? I certainly hope so, but let's analyze exactly what this drug does in its present state: The drug still resulted in almost 30% of the patients experiencing a 70% increase in permeability (leaky gut) – Not good. A highly pro-inflammatory (this means that it creates degenerative disease) substance known as interferon gamma was also produced in nearly 30% of the drug-consuming patients tested – Not good. Leakiness, or the passage of negative substances through cells is not affected by this drug – Not good. Of course on the plus side, over 70% of those tested DID have a very good result with apparently no untoward side effects – Very good. At what point is the efficacy high enough that you'd be willing to subject yourself to a possible reaction? Do realize that any gluten ingested increases your chance of disease, chief amongst them cancer and autoimmune disease. Is there a level of function of the drug that you would chance taking it? Is it 90%, 99%? Does any drug ever get that good? Well, as a big fan of Dr. Fasano's, I would say that if anyone can do it, he and his team can. But at the same time, I cannot help but think of all the other drugs I have encountered. As 'wonderful' as they sometimes seem initially, they almost always fall from grace when some horrible side effect is realized. Would I guinea pig my own health that I've fought so hard to regain? Would I recommend taking such a chance to my children just so that they could consume some white flour product? I don't think so. How about you? What do you think? If the drug were available right now at its efficacy of 71%, would you take it and hope you weren't in the 29% for whom it didn't work? I'd love to hear your thoughts. If you are wondering if you're gluten intolerant or know that you are but still aren't enjoying good health, consider calling us for a free health analysis: 408-733-0400. We are here to help! Our destination clinic sees patients from across the country and internationally so you do not need to live locally to receive assistance. To your good health! Reference: Alessio Fasano, Clinical and Developmental Immunology, Published online 2012 October 10. "Novel Therapeutic/Integrative Approaches for Celiac Disease and Dermatitis Herpetiformis." -
Celiac.com 08/21/2015 - Here's every celiac disease treatment currently in development in a single list: ALV003, by Alvine Pharmaceuticals, is a combination of two enzymes that break down gluten before it can provoke an immune reaction. The drug is a powder to be dissolved in water and taken before meals. ALV003 most recently passed a phase 2 clinical trial, results of which appeared in the June 2014 issue of Gastroenterology. Post-trial biopsies showed that ALV003 prevented intestinal damage in 34 volunteers with celiac disease who ate 2 grams of gluten each day for six weeks and also took the drug. Phase 2b, a 12-week trial, is now underway. AN-PEP, by DSM Food Specialties, is another enzyme that degrades gluten. AN-PEP is believed to work best when taken while gluten is still in the stomach. Results from a small 2013 study showing AN-PEP to be safe, appeared in the World Journal of Gastroenterology. For the study, 16 people ate 7 grams of gluten every day for two weeks and half of them also ate AN-PEP, and half took a placebo. However, the placebo group did not get sick enough during the course of the study to show that the enzyme had any effect, so further study is under way. ActoBiotics by ActoGenX uses Lactococcus lactis as an expression system to locally secrete bio-therapeutics such as cytokines, antibodies, hormones, etc. Early pre-clinical work with a genetically altered L. lactis secreting a peptide derived from gliadin demonstrated an in vivo suppression of gluten sensitization. Specifically, Huigbregtse et al. engineered L. lactis to secrete a deamidated DQ8 gliadin epitope (LL-eDQ8d) and studied the induction of Ag-specific tolerance in NOD ABo DQ8 transgenic mice [34]. Although apparently not part of the ActoGenX development program, recent work by Galipeau et al. also deserves mention in this context. The group treated gluten-sensitive mice with elafin, a serine protease inhibitor, delivered by the L. lactis vector, and found normalization of inflammation, improved permeability, and maintained ZO-1 expression. There is speculation that this is due to reduced deamidation of gliadin peptide. AVX176 by Avaxia Biologics, is an investigational oral antibody drug patented to provide "Antibody Therapy for Treatment of Diseases Associated with Gluten Intolerance." The patent, which expires on May 27 2029, provides broad coverage for treating celiac disease using orally administered antibodies produced by Avaxia's proprietary platform technology. BL-7010, by BioLineRx, is a novel co-polymer for the treatment of celiac disease, which significantly reduces the immune response triggered by gluten. This drug has been shown in mice to reduce the immune system response that leads to intestinal damage and villous atrophy in celiac disease. BL-7010 actually binds to the gluten protein, reducing the protein's toxicity.The drug, with the gluten molecule attached, then passes harmlessly through the digestive system to be expelled as stool. BL-7010 has undergone safety testing in humans and was found to be well tolerated. According to BioLineRx, testing will begin in mid-2015 to see if the drug works as expected to diminish gluten's effects on the body. However, BL-7010 is designed to protect only against gluten cross-contamination; it won't allow people with celiac disease to eat large amounts of gluten. CCR9, by Chemocentryx, is a drug called vercirnon, which is also known as Traficet-EN, or CCX282B), and was originally intended for patients with moderate-to-severe Crohn's disease. CCR9 has completed one Phase 2 trial in 67 patients with celiac disease. However, despite the completion of the trial several years ago, no results relating to celiac disease have been made public or published. Egg Yolk Enzyme. Little is known about efforts to develop a celiac treatment that uses egg yolk to coat gluten and allow it to pass through the body undetected, thus preventing an adverse gluten reaction in sensitive individuals. Like most other drugs being developed, this treatment would work to prevent reactions to small amounts of gluten, rather than as a cure. Larazotide Acetate by Alba Therapeutics. How it works: Larazotide acetate blocks a protein that carries pieces of gluten across the gut, where immune cells can see them. Fasano and his colleagues found that this carrier protein, called zonulin, is overproduced by celiac patients after they eat gluten. Results of the most recent phase 2 trial of larazotide acetate, published in February 2015 in Gastroenterology. The volunteers who took the drug experienced fewer days with disease symptoms during the 12 week-long study. Nexvax2, by ImmusanT, works much like an allergy shot. Nexvax2 exposes the immune system to gluten in a controlled way so that immune cells that are usually activated get turned off or eliminated. So far, Nexvax2 has completed a phase 1 trial showing it to be safe. More research is being done to test whether it is effective. Designed to work as a vaccine, Nexvax2 combines three proprietary peptides that elicit an immune response in celiac disease patients who carry the immune recognition gene HLA-DQ2. Similar to allergy shots, the vaccine is designed to reprogram gluten-specific T cells triggered by the patient's immune response to the protein. ZED1227 by Dr. Falk Pharma and Zedira recently announced the start of phase I clinical trials for the drug candidate ZED1227, a direct acting inhibitor of tissue transglutaminase. The small molecule targets the dysregulated transglutaminase within the small intestine in order to dampen the immune response to gluten which drives the disease process. Stay tuned for updates and progress reports as these drugs work their way through their various trial phases. Finally, share your thoughts on all these celiac drugs in the development pipeline. Are you excited, wary, both? Let us know by commenting below. Source: Gastroenterology Report
- 26 comments
-
- celiac
- celiac disease
-
(and 5 more)
Tagged with:
-
Celiac.com 09/06/2019 (Originally published 04/05/2010) - I have a mental calendar that outlines some of the major contributors to the celiac community. It is a limited one, as I can not list all of the many thousands of contributors to our community. But I think I am aware of some of the most prominent of these, beginning with the discovery of the efficacy of the gluten free diet. In the 1930s, the most significant insight into celiac disease came from Dr. Willem Karel Dicke, a towering giant in the field of celiac research. His contribution of the gluten-free diet is the single most powerful contribution to the celiac community that has ever been made. Although others expressed insight into this condition, Dr. Dicke serves, in my mind, as the starting point for a modern understanding of celiac disease and gluten sensitivity. We cannot guess just how long it might have taken before some other pediatrician or gastroenterologist listened to the insightful comments of a concerned mother who had noticed that her child’s skin rash (possibly dermatitis herpetiformis) resolved when wheat was removed from the child’s diet. Please pause for a moment to think about this. Even seventy five years after Dr. Dicke’s discovery, would your physician, or your child’s pediatrician, investigate a nutritional theory you offered him or her? I think very highly of her, but I’m not sure that my physician would do so. The fact that Dr. Dicke listened that carefully to this concerned mother is the springboard that vaulted him to what I believe is the single greatest achievement in the history of celiac disease. By the 1950s, after Dr. Dicke’s thesis was published, the Crosby capsule was developed by Dr. William H. Crosby and was a major step forward for taking endoscopic biopsies from the small intestine. It may have been a mixed blessing though. While it identified some patients with severe, widespread villous atrophy, it likely missed most cases of celiac disease. During those early years, a gluten free diet was considered an extreme dietary measure and was usually not recommended unless celiac disease could be confirmed. Many physicians continue to see the diet in that light. Fortunately, that paradigm is changing, both through the improved quality and distribution of gluten free foods along with the trend of more and more health care professionals coming to realize some of the many benefits and the reduced burden of following a gluten free diet. In the 1960s, Dr. Curtis Dohan was the first to test the hypothesis that gluten might be a factor in schizophrenia – perhaps appreciating that LSD, taken by many Psychology and Psychiatry students at that time to mimic the experience of the schizophrenic, is refined from the mold that grows on gluten grains. He pointed to similarities between the indoles found in the urine of schizophrenics and those found in gluten grains. He went on to conduct research and publish his findings along these lines for more than two decades. His publications would prove prophetic even among those who had previously disparaged his work, as we now know that many schizophrenics mount immune responses to gluten that are usually quite dissimilar to those found in most celiac patients. Nonetheless, the evidence of gluten as a factor in schizophrenia has now been established by several different approaches conducted by several different groups. As Dr. Dohan was conducting his first research in this area, one of the most enduring and important figures in Twentieth Century celiac research entered the arena. Dr. Michael N. Marsh began his illustrious career in medicine with his graduation from the University of Leeds, School of Medicine in 1960. After a brief foray into obstetrics, he specialized in gastroenterology and dedicated most of the next 40 years to sub-specialty research on celiac disease. His work unveiled many facets of the immunological reactions to gluten inherent in celiac disease which provided a foundation for many subsequent advances in celiac research that followed. He developed the rectal challenge protocol which, although it continues to be experimental, is probably the best single test for identifying celiac disease and only celiac disease. As if that were not enough, he also developed the Marsh system to aid pathologists in categorizing the various forms of altered villous morphology that are consistent with celiac disease. Dr. Marsh’s retirement in 2000 was a loss to every celiac patient on the planet. Although he went on to publish another book about celiac disease and write and publish several more papers before he shifted to the pursuit of yet another doctoral degree (his fourth by North American standards). In 1984, Doctors Cooke and Holmes, contemporaries of Marsh, compiled a compelling medical textbook. Coeliac Disease may have been the first medical textbook devoted exclusively to celiac disease. It owns a special place in my heart because it is so well written that I found the information quite accessible even when I first began to explore the literature on celiac disease. These venerable gastroenterologists continued to conduct original research and thoughtful commentary both in the literature and at conferences. In the same decade, Dr. Martin Kagnoff was, I believe, the first to suggest that exposure to viral agents (specifically adenovirus 12) in addition to the predisposing HLA genetic markers, might be the key difference between those with the genetic predisposition who did and did not develop celiac disease. Several investigations have since explored exposure to other viral agents, with varying degrees of success. Also in the 1980s, both doctors Paul and Kozlowska each published separate accounts, in German and Polish respectively, of celiac children. About 70% of these youngsters showed signs and symptoms that are diagnostic for attention deficit disorders (ADD) but these criteria went away after six months to a year of strict compliance with a gluten-free diet. Again, in the 1980s, Dr. Vijay Kumar was an early pioneer in the development of antibody testing for celiac disease. Early in the 1990s, Dr. Carlo Catassi pioneered the use of endomysium antibody tests to conduct large screening studies for celiac disease among children throughout entire school districts in Italy. He first revealed high rates of celiac disease in Italy, of 1:250 (a startling number at that time) then in Sub-Saharan Africa where 5.6% of Saharawi children were shown to have celiac disease. These findings served as a template for similar work conducted in the USA. It was spearheaded by a group of researchers including Dr. Alessio Fasano, Dr. Peter Green, and several others at medical centers across the US. These same individuals have done wonders for celiac awareness in North America. Also in the 1990s, Dr. Kenneth Fine raised an early and strong voice in recognition of non-celiac gluten sensitivities. His voice continues to echo through the celiac and gluten sensitive community, as his laboratory continues to test for fecal antibodies against gluten. By the mid 1990s, Dr. Marios Hadjivassiliou had pioneered many facets of gluten-induced neurological disease, raising the alarm that more than half of neurological disease of unknown origin is associated with gluten sensitivity. And in 1997, Dr. A. De Santis and associates showed smoking-gun evidence on SPECT scans, that removal of gluten from the diet of at least one schizophrenic returned the patient to normal blood distribution in the brain, and normal behaviour. From the 1980s and continuing into today, Dr. Rodney Ford, a long time advocate of the gluten free diet for many associated conditions, first conceptualized the notion that celiac disease may begin as a neurological condition and only a subset of those whose nerves are injured by gluten will go on to develop villous atrophy. Further to the work of Hadjivassilou, Fine, Paul, Kozlowska, and Dohan, he has gone on to work on teasing out information from his patients and their records to show the gluten free diet can provide substantial academic and social benefits to these children. In the 1990s Dr. Joseph Murray added some startling examples to the long list of anecdotal reports of anomalous, overweight celiac patients. Near the end of that decade Dr. William Dickey investigated this issue and found that while 22% of one group of celiac patients were underweight, 34% were overweight, and the remainder fell somewhere in the normal range. Thus, only a minority of Dr. Dickey’s patients fit the malnourished and wasting stereotype often associated with celiac disease. His data demonstrate that the possibility of celiac disease should not be dismissed on the basis of body mass index when working with normal, overweight, and obese patients. No discussion of heroes of the celiac community would be complete without further mention of Dr. Alessio Fasano and his work. As previously mentioned, he has contributed enormously to celiac awareness. However he and his lab associates also discovered and characterized zonulin, a major mediating factor of intestinal permeability. He is also involved in the subsequent development of Larazotide, a drug that permits celiac patients to consume gluten with little or no adverse effects. Celiac awareness is growing rapidly in the US and Canada. Celiac and gluten sensitive patients have great cause for optimism as these many paths of research continue to open up. However, much of that work is not yet complete. Two people I know well have recently been diagnosed with pernicious anemia, yet neither of the attending physicians has even suggested testing for celiac disease. However, the future is full of promise for our children and their children. Enormous strides are being made in building awareness (celiac disease is commonly in the media now) and more and more physicians and patients are increasingly aware of celiac disease and it is being diagnosed much more frequently with every passing year. That’s where we’ve been. But where are we going? Has awareness built to critical mass where it will be self sustaining? It is hard to say. But so many of those diagnosed with celiac disease believe, as I do, that we should have been diagnosed much earlier, if only the doctors had listened to what we were telling them. We are understandably anxious to see this trend of overlooking celiac disease come to an end. Each of us, in our own way, continues to push celiac awareness and as long as this is happening, I think we can assume that the trend toward increasing celiac awareness will be self sustaining, at least in the short term. It may also be fair to suggest that through increasing celiac awareness and the resulting reduction in delays to diagnosis, there will be fewer celiac-related cancers and autoimmune diseases arising out of untreated celiac disease. Increased awareness is also making more gluten-free foods more widely available. And economies of scale should eventually bring down the price of these food items. In all, earlier diagnosis should lead to increased life expectancies and improved quality of life for younger generations of celiac patients. But those gains are only the tip of the iceberg. Increased rates of diagnosis should lead to fewer children struggling in school, greater general nutritional awareness. Larazotide or its derivatives will keep us safe when dining in risky places. More than half of neurological diseases of unknown origin may become preventable and more treatable. Some mental illnesses may prove to be more treatable on a gluten free diet. The current status of celiac awareness and available therapies gives good cause for optimism. The future is looking better too. 2009 saw a multi-author publication identifying non-celiac immune reactions in schizophrenic patients. Two years earlier, we saw a report by Anderson et al. that indicated higher rates of cancer and death among those with non-celiac gluten sensitivity than among those with celiac disease. The tide is turning. Non-celiac gluten sensitivity is clearly beginning to get some attention as a serious condition in its own right. This augurs well for increasing awareness of gluten sensitivity. Since this group forms 10 to 12 percent of the general population, and if studies of this sort continue to be conducted, we may soon see exponential gains in gluten free options. Perhaps a cultural shift away from gluten grains is a possibility. Both groups that conducted these investigations may someday be recognized as heroes for their willingness to investigate these questions. We may soon see a day when gluten free wheat is used to make bread that is safe to eat for all of us. That research has been under way in Germany for quite some time. Similar efforts are under way in the US. The future may also see the development of digestive enzymes that, when taken with gluten, will break the bonds that bind the harmful peptides in gluten. All of the above are very worthy goals. But there is a vastly greater benefit that is currently growing in our midst. There is a sense of connection and belonging that each of us feels when we encounter another person who also avoids gluten to improve or preserve their health. We are forging an international fellowship that knows no racial, economic, or social barrier. Our common bond is our shared journey through a gluten-infested labyrinth that shapes our food supply. And we feel a sense of affinity which may be one of Humanity’s most important needs. This sense of kinship arises in the context of support groups, listservs, commercial enterprises that serve our needs and day-to-day encounters in our communities. We are a growing fellowship of gluten avoiders.
-
- celiac
- celiac disease
-
(and 4 more)
Tagged with:
-
On the contrary, many celiacs spend decades feeling unhealthy even though they are on 100% gluten-free diets, and many are even on grain-free and other very restrictive diets. Some feel like they are going crazy and cannot even venture outside or do any travel without bringing their own food. This "alarming" headline is for those celiacs who are not recovering on a gluten-free diet, and it is alarming because the results of this study are alarming. Many celiacs simply won't recover on the gluten-free diet, and will likely need additional treatment to deal with the disease. What treatment that will be remains to be seen. Will it be Larazotide Acetate? Will there be genetic or other tests to determine which celiacs won't recover on a GFD? If you fall into the category of people in this study who will not recover by diet alone, you may also find its results alarming.
- 19 comments
-
- celiac
- celiac disease
-
(and 5 more)
Tagged with:
-

The Media Encourages Negative Social Behavior Towards Gluten-Free Dieters
Guest commented on Jean Duane PhD's article in Winter 2018 Issue
Just wait about 3 years. The drug larazotide acetate is expected to go into Clinical trial level 3 this year (2nd quarter of 2018). The drug is expected to stay in level 3 for 3 years. It's expected to go into Clinical trial level 4 after that. Level 4 is when the drug is given to doctors to give to the applicable general public. The drug is supposed to help people with celiac disease. Larazotide acetate counteracts the effects of the hormone zonulin. When the drug enters level 4 expect to be inundated with ads everywhere telling people to get tested for celiac disease. I'm thinking that the drug will be able to be used for people with non-celiac gluten sensitivity (NCGS), too. I suspect that the medical industry will come out with a blood test for NCGS in 3 years, too.- 15 comments
-
- behavior
- gluten-free diet
-
(and 4 more)
Tagged with:
-
Celiac.com 03/12/2010 - According to the National Institutes of Health, approximately 3 million Americans suffer from celiac disease. Characterized by small intestinal inflammation, intestinal injury and intolerance to gluten, celiac is a genetic T-cell mediated auto-immune disease. Those diagnosed with celiac disease know that the only cure is an entirely gluten-free diet for life. When left untreated, celiac can manifest into life-threatening illnesses such as, heart disease, osteoporosis, and cancer. However, modern science is now presenting us with an alternative to suffering needlessly, and it comes in the shape of a little non-assuming pill called Larazotide Acetate. While celiac disease affects 1 in 133 people, those numbers do not take into account the thousands of other people who are impacted from gluten intolerance and gluten related allergies. Gluten comes in many disguises but can be found primarily in wheat, rye, and barley. Since the Food and Drug Administration has not yet mandated gluten disclosures on labels, many foods are contaminated with hidden gluten. People that suffer from the inability to digest gluten are extremely limited when it comes to dining, and often find themselves eating alone or bringing their own gluten-free food to social events. Eating a microscopic amount of gluten, for many gluten sensitive sufferers, frequently leads to varying degrees of sicknesses including, diarrhea, vomiting, rashes, and insomnia. Some people are more sensitive than others, and those most sensitive to gluten cannot eat at many restaurants due to the chance of cross contamination. Much like a peanut allergy, those gluten sensitive can get sick from eating gluten-free food that was cooked in the same kitchen as gluten food by means of contamination, or simply from receiving a kiss from a loved one that has traces of gluten on their mouth. With so many unsavory reactions to food, the medical community has been attempting to devise a drug for celiacs that allows them to safely digest gluten. A new drug called Larazotide Acetate, has been called 'revolutionary' to the celiac and gluten sensitive community, and may be what celiacs need to live a more normal life. While it is not a cure, Larazotide Acetate has been proven in clinical trials to greatly reduce the negative reactions celiacs have with gluten. Clinical test patients displayed a decrease in intestinal damage, from 50% to 15%, when ingesting gluten after taking Larazotide Acetate. Larazotide Acetate may very well be the new breakthrough drug of the decade. It offers celiacs and others with gluten sensitivities, the freedom to eat out at restaurants, or go to a friends house for dinner without the physiological and emotional stress that can accrue from worrying about, and getting sick from gluten contaminated food. Source: http://calgary.ctv.ca/servlet/an/local/CTVNews/20100305/edm_gluten_100305/20100305/?hub=CalgaryHome
- 8 comments
-
- celiac
- celiac disease
-
(and 2 more)
Tagged with:
-
Celiac.com 12/16/2014 - Will people with celiac disease spend money on drugs designed to reduce or eliminate adverse reactions to gluten? Drug researchers and investors are betting they will. Currently, the only proven treatment for celiac disease is a strict gluten-free diet. However, a number of companies are looking to debut drugs for treating celiac disease in the next five years, With that in mind, Abhilok Garg, Ph.D., an immunology analyst with research and consulting firm GlobalData, is projecting sales such drugs in the US and five major European markets Germany, France, Spain, Italy and the UK, to reach approximately $551.1 million by 2023. The launches of Alba/Teva’s larazotide acetate, Alvine/AbbVie’s latiglutenase, and BioLineRX’s BL-7010 portend a new world of therapies for the estimated 600,000 diagnosed celiac patients in these countries. With early trials looking promising and no obvious problems on the horizon, analysts expect larazotide acetate to enter the US and 5EU markets in Q1 2018 and Q1 2019, respectively, followed by latiglutenase in Q1 2019 and Q1 2020. Latiglutenase is currently being developed as a chronic drug treatment, GlobalData’s interviews with KOLs have indicated that clinical experience with this drug could dictate the way it is prescribed to patients, and that it may in some cases be used as an “on demand” treatment,” says Dr. Garg. Larazotide acetate works by modulating tight junctions (TJs) in the small bowel epithelium, and has tried to maximize recent research showing that people with celiac disease do have altered intracellular spaces and TJ structures in the lower esophagus. BL-7010 works by sequestering gliadins, effectively masking them from enzymatic degradation and preventing the formation of immunogenic peptides that trigger an adverse immune reaction when people with celiac disease consume wheat. BL-7010 has cleared early trial hurdles and been found to be safe and well tolerated in both single and repeated-dose administrations. Does the idea of a reliable treatment for celiac disease appeal to you? Would you try such drugs, or just stick with the gluten-free diet? Source: Pharmabiz.com
-
Celiac.com 07/28/2014 - One angle being tried by researchers to treat celiac disease involves oral peptides. These are orally administered drugs that would prevent an adverse gluten reaction in people with celiac disease who are following a gluten-free diet. The drugs are intended to prevent adverse reactions from minor gluten contamination or exposure. In a recent update from the Mayo clinic, Joseph Murray, MD, confirms that larazotide acetate, a first-in-class oral peptide, has ”met the study's primary end point of a reduction in GI symptoms.” Dr. Murray presented the results from the study as a late-breaking abstract at Digestive Disease Week 2014. In a celiac disease reaction, the epithelial tight junctions that control paracellular permeability are compromised, and gut permeability increases. This is partly due to an inflammatory immune response to the entrance of gluten peptides into the intestinal lamina propria through these tight junctions. Larazotide acetate prevents tight-junction opening and reduces gluten uptake, inhibiting gluten- and cytokine-induced intestinal permeability and inflammation in vivo. This randomized, parallel, double-blind, placebo-controlled, multicenter trial was conducted at 74 sites in North America. The aim was to evaluate the effect of larazotide acetate on GI signs and symptoms in patients with celiac disease. Source: Medscape.com