
1.3 Drug-resistant TB
Since 1994, the World Health Organization (WHO) has systematically collected and analysed data on levels of resistance to anti-TB drugs from countries and areas (1). Most attention has been given to the proportion of people diagnosed with TB who have rifampicin-resistant TB (RR-TB) and multidrug-resistant TB (MDR-TB, defined as resistance to both rifampicin and isoniazid), collectively referred to as MDR/RR-TB (for data sources and availability, see Box 1.3.1). Since 2022, new methods have been used to produce time series of estimates of the number of people developing MDR/RR-TB each year (incident cases), covering the period from 2015 up to the most recent complete calendar year (2, 3). Data on resistance to other anti-TB drugs are collected as well, but the country coverage of such data is much more limited.
Globally, the estimated annual number of people who developed MDR/RR-TB was relatively stable between 2020 and 2022, after a slow downward trend between 2015 and 2019 (Fig. 1.3.1). The estimated number in 2022 was 410 000 (95% uncertainty interval [UI]: 370 000–450 000). Compared with the time series published in the Global Tuberculosis Report 2022 (4), there was a downward revision for all years since 2015, for two main reasons: downward revisions to overall estimates of TB incidence (Section 1.1); and revisions to estimates of the proportion of people with TB who had MDR/RR-TB in several countries, most notably Pakistan (details are provided in Annex 5 of the main report).
Globally, MDR/RR-TB caused an estimated 160 000 (95% UI: 98 000–220 000) deaths in 2022.
The reason why the number of people developing MDR/RR-TB is not estimated to have increased from 2020–2022, in contrast to the number of people developing TB overall (Section 1.1), is that increases in the overall number of people developing TB have been compensated for by an estimated downward trend (since 2015) in the proportion of people with TB who have MDR/RR-TB, particularly among those with a previous history of treatment (Fig. 1.3.2).
Globally, the estimated proportion of new TB cases with MDR/RR-TB fell from 4.0% (95% UI: 3.1–4.9%) in 2015 to 3.3% (95% UI: 2.6–4.0%) in 2022; the estimated proportion of previously treated cases with MDR/RR-TB was 25% (95% UI: 15–36%) in 2015 and 17% (95% UI: 11–23%) in 2022.
Trends at regional level vary (Fig. 1.3.3). Between 2020 and 2022, there were estimated increases in the number of people who developed MDR/RR-TB in two WHO regions (the Americas and South-East Asia), in contrast to continued slow declines in the African, Eastern Mediterranean and Western Pacific regions and declines from 2015–2020 and 2021–2022 in the European Region.
Trends in the 30 high MDR/RR-TB burden countries also vary (Fig. 1.3.4).
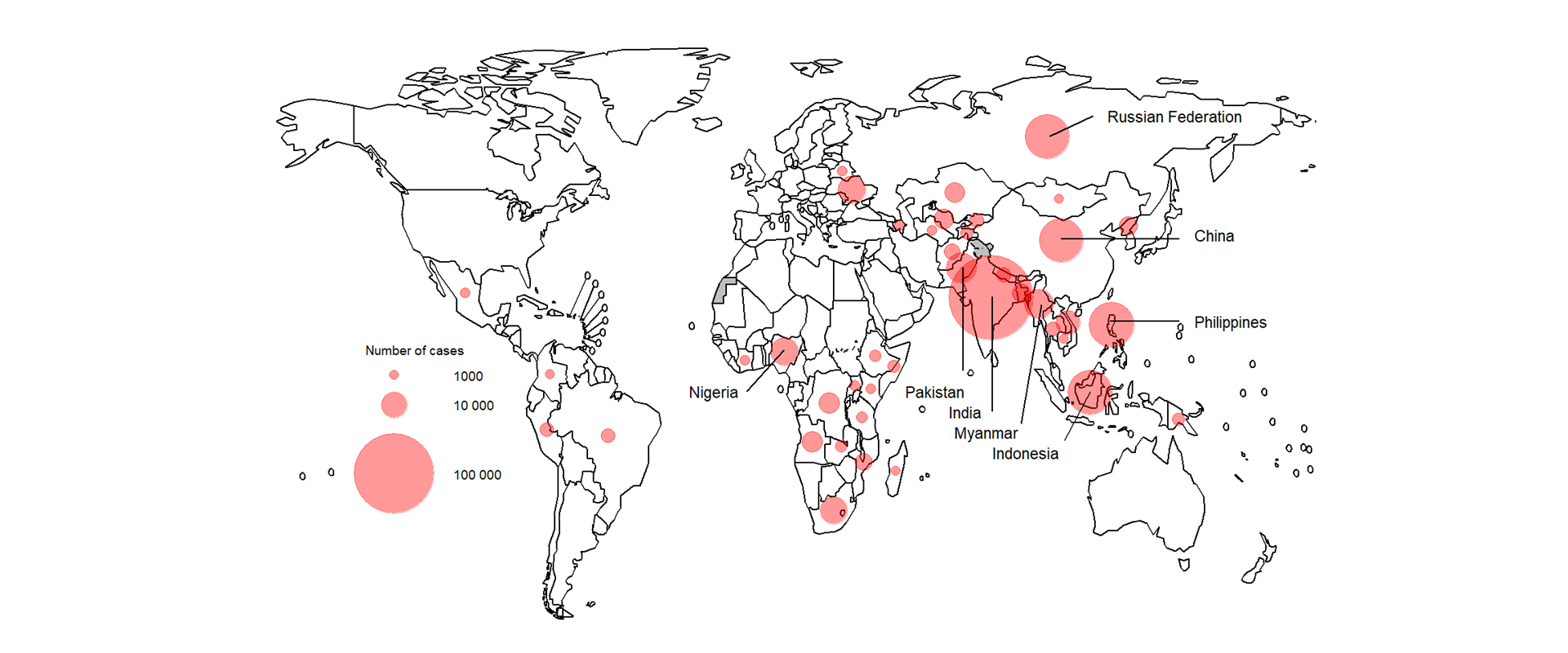
The countries with the largest share of the global number of people estimated to have developed MDR/RR-TB (incident cases) in 2022 were India (27% of global cases), the Philippines (7.5% of global cases) and the Russian Federation (7.5% of global cases) (Fig. 1.3.5).
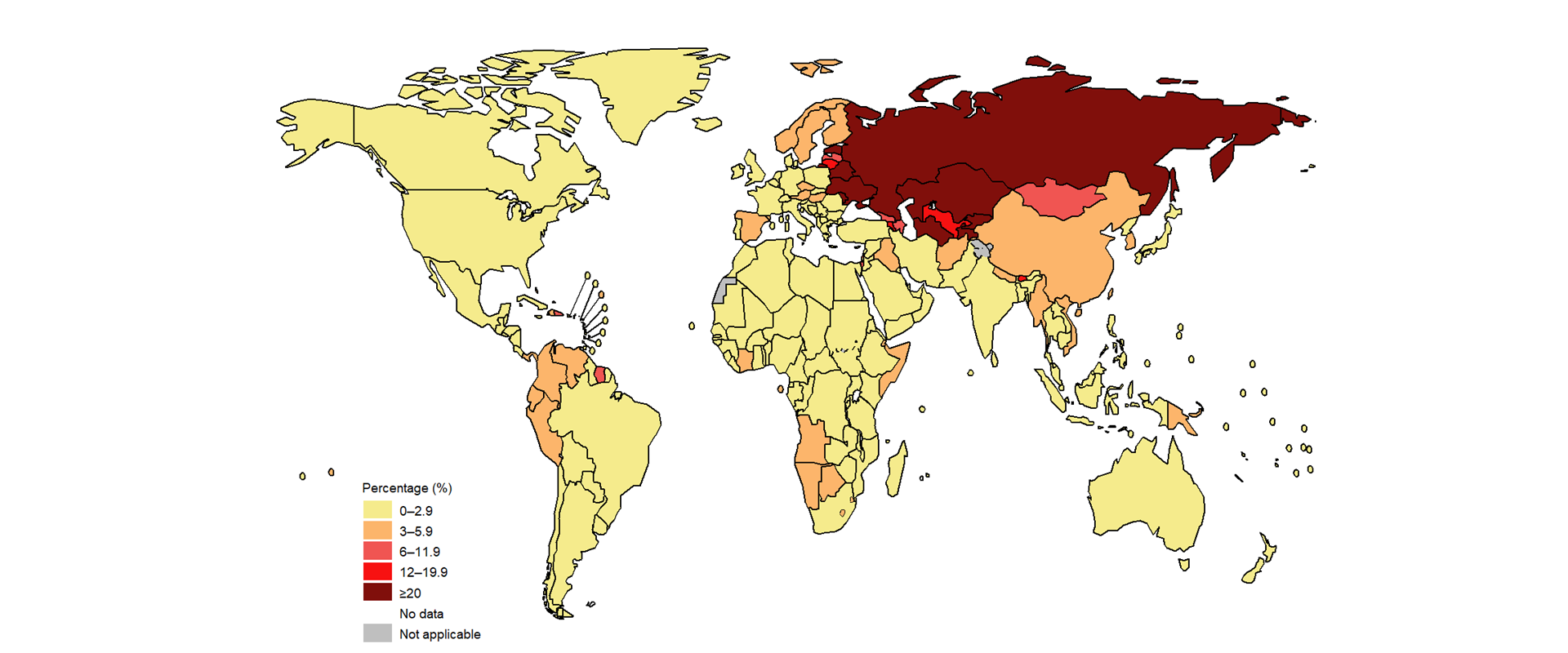
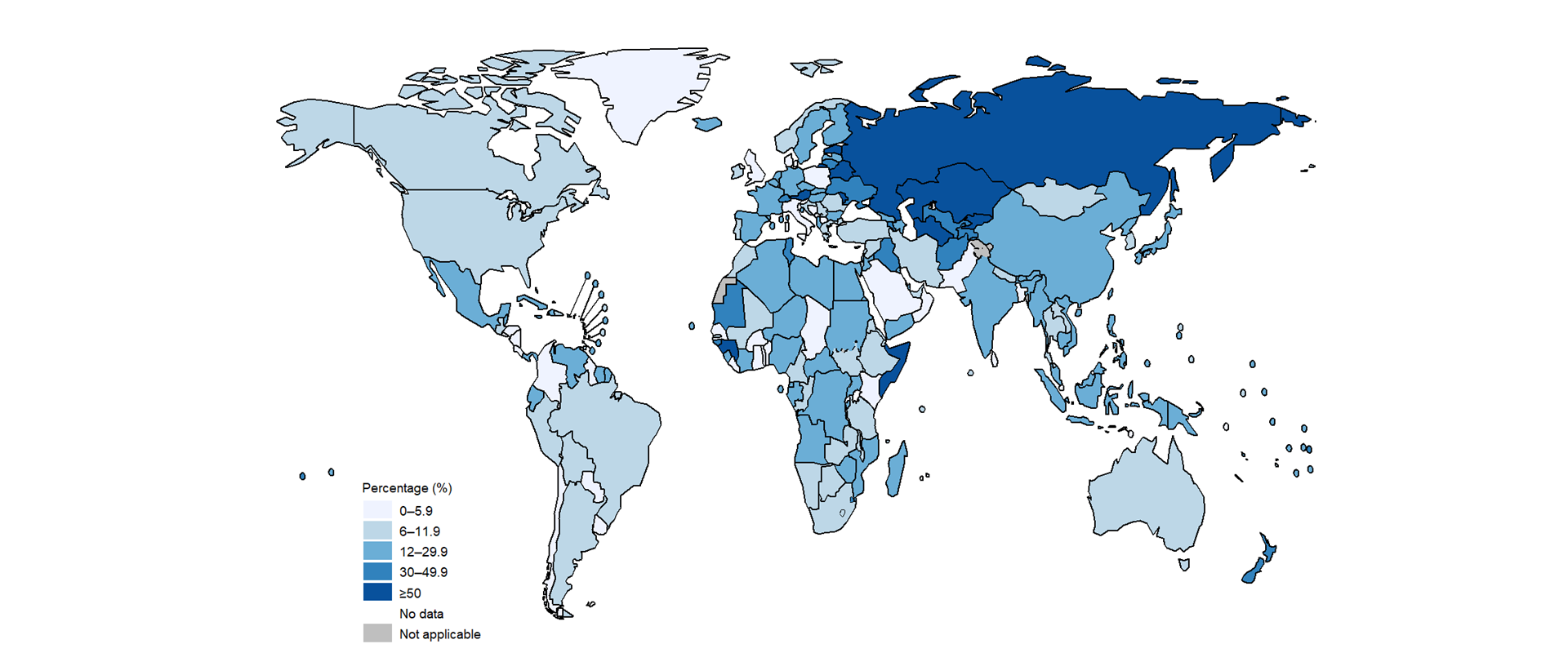
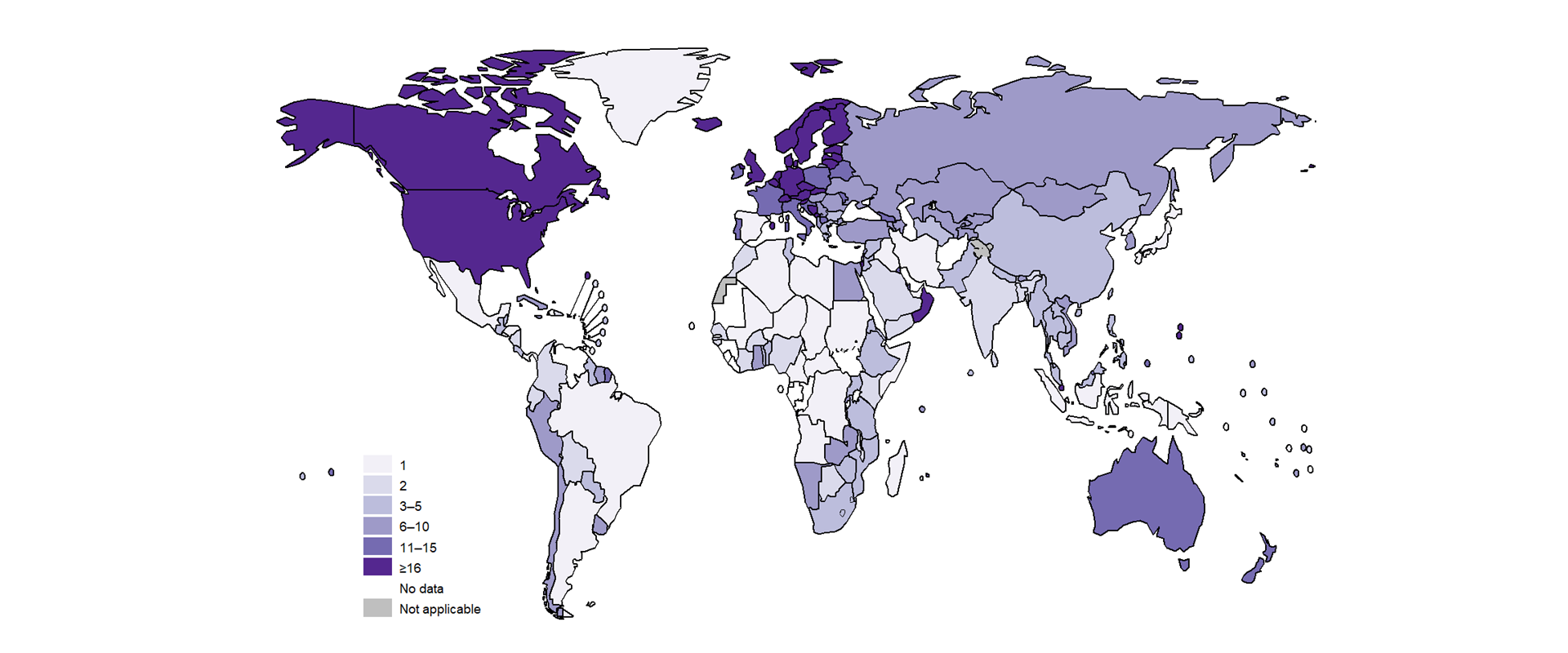
The proportion of people with TB who had MDR/RR-TB varies considerably among regions and countries (Fig. 1.3.6, Fig. 1.3.7). For people with no previous history of TB treatment (new cases), best estimates range from less than 3% in the WHO African, South-East Asia and Eastern Mediterranean regions to 24% in the European Region. For people previously treated for TB, best estimates range from 8.4% in the Eastern Mediterranean Region to 54% in the European Region. At country level, the highest proportions are found in the Russian Federation and in several countries in eastern Europe and Central Asia.
Other patterns of drug resistance
There were an estimated 1.3 million incident cases (95% UI: 0.39–2.3 million) of isoniazid-resistant TB in 2022, including people with both rifampicin-susceptible and rifampicin-resistant TB.
Globally in 2022, the estimated proportion of MDR/RR-TB cases with pre-XDR TB (i.e. resistance to any fluoroquinolone for which testing was done) was 18% (95% CI: 16–20%).
Box 1.3.1: Anti-TB drug resistance: data sources and availability
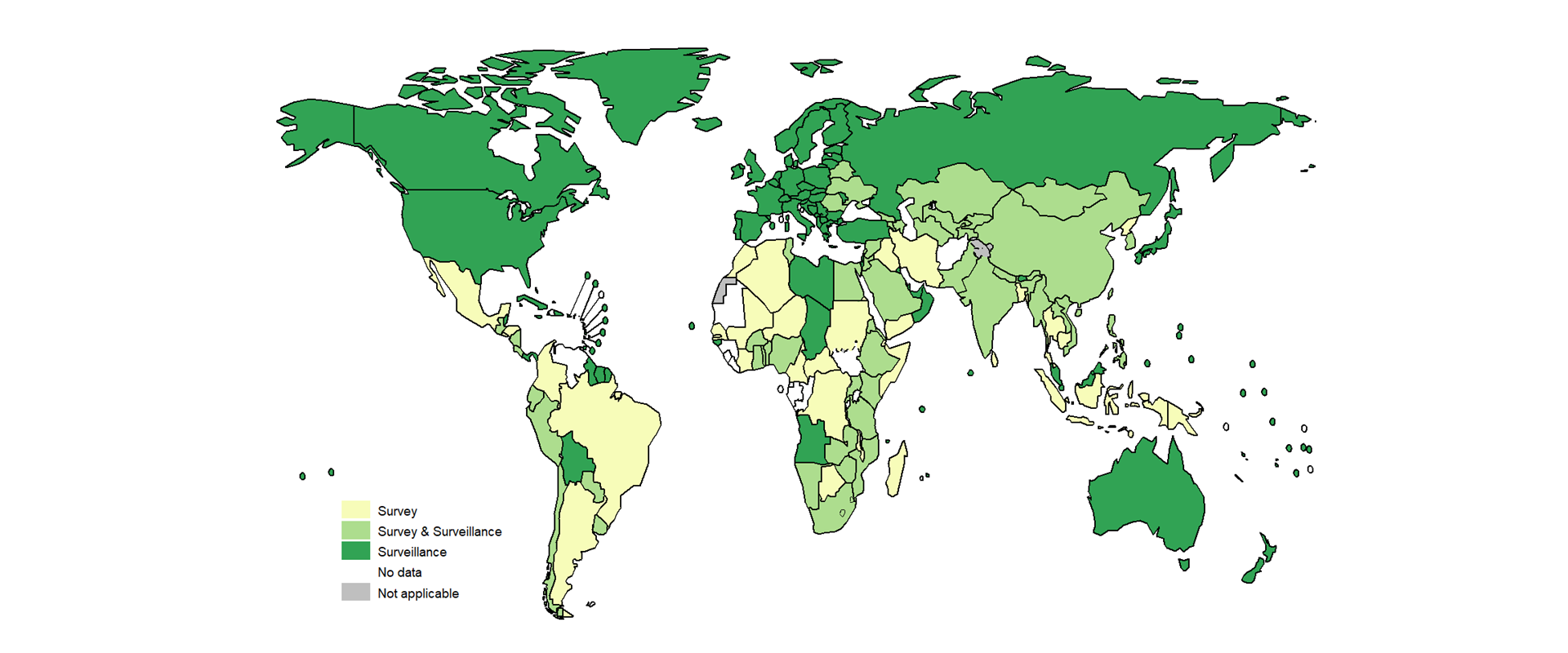
There are two main sources of data about levels of anti-TB drug resistance: national surveys and continuous surveillance (i.e. routine diagnostic testing for drug resistance among people diagnosed with bacteriologically confirmed TB) (5).
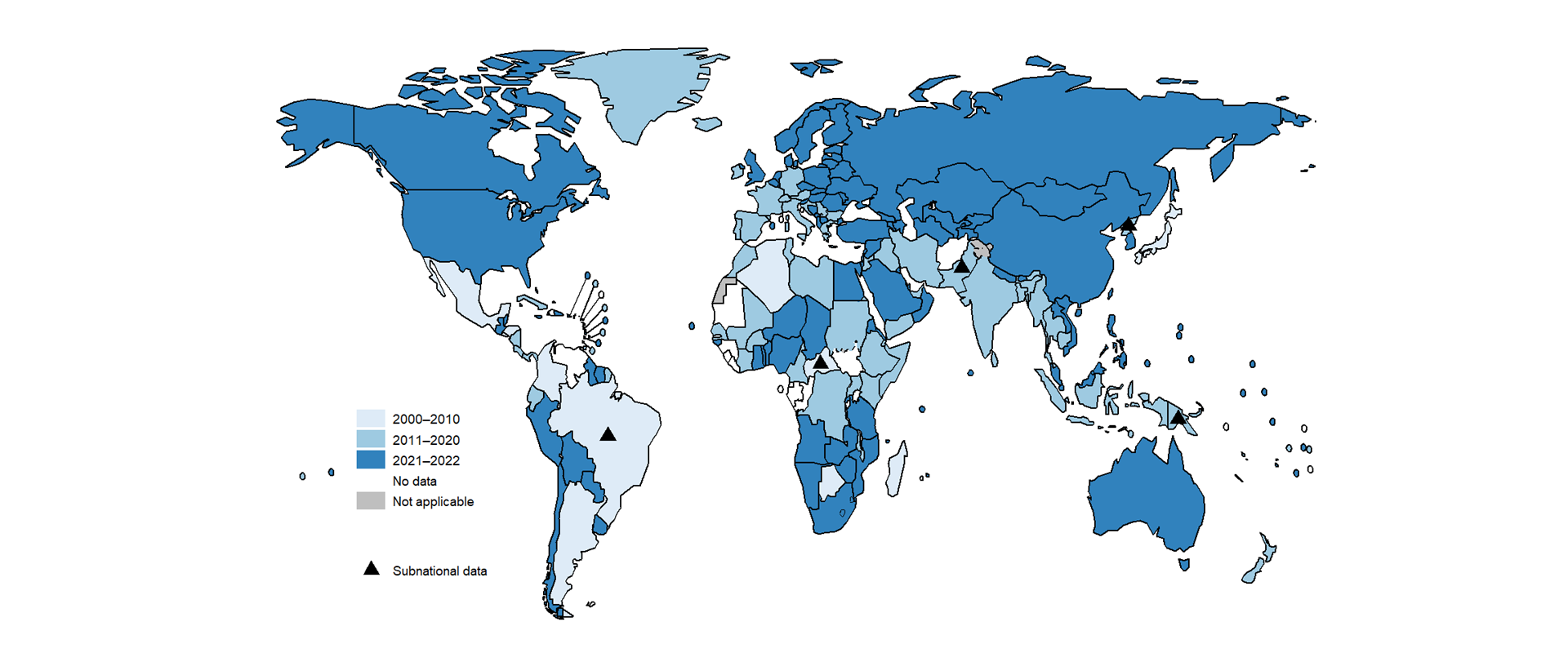
As of August 2023, 105 countries and areas had representative data about levels of resistance to rifampicin from continuous surveillance systems, 33 had nationally-representative survey data dating from 2000 or later and 53 had data from both continuous surveillance and surveys (Fig. 1.3.8, Fig. 1.3.9, Fig. 1.3.10). This total of 191 countries and areas worldwide collectively accounted for 98% of the world’s population and 98% of incident cases of TB in 2022.
Of the 43 countries that are in one or both lists of high TB burden and high MDR/RR-TB burden countries being used by WHO in the period 2021–2025, 40 had survey or surveillance data on levels of drug resistance.
References
Dean AS, Tosas Auguet O, Glaziou P, Zignol M, Ismail N, Kasaeva T et al (2022). 25 years of surveillance of drug-resistant tuberculosis: achievements, challenges, and way forward. Lancet Infect Dis 22(7):E191-E196 (https://doi.org/10.1016/S1473-3099(21)00808-2).
WHO Global Task Force on TB Impact Measurement: report of a subgroup meeting on methods used by WHO to estimate TB disease burden, 11-12 May 2022, Geneva, Switzerland. Geneva: World Health Organization; 2022 (https://iris.who.int/handle/10665/363428).
Background document 2. Methods for estimating the incidence of drug-resistant TB. In: WHO/Global Task Force on TB Impact measurement [website]. Geneva: World Health Organization; 2022 (https://cdn.who.int/media/docs/default-source/hq-tuberculosis/global-task-force-on-tb-impact-measurement/meetings/2022-05/tf-2022-05-2-background--document-2--dr-tb.pdf?sfvrsn=a8757cfa_3).
Global tuberculosis report 2022. Geneva: World Health Organization; 2022 (https://iris.who.int/handle/10665/363752).
Guidance for the surveillance of drug resistance in tuberculosis: Sixth edition. Geneva: World Health Organization; 2020 (https://iris.who.int/handle/10665/339760).
